Vaccination
Vaccines are key in making progress against infectious diseases and save millions of lives every year.
This article was first published in July 2015, and last revised in February 2024.
Vaccines are technologies that help protect people against developing diseases. Since the invention of the first vaccine, against smallpox, vaccines have greatly reduced the prevalence of diseases everywhere in the world.
This page describes which vaccines are available and where they are used, what their impact on global health is, and how the world can make more progress against early death and disease with the help of vaccines.
We thank Stephanie Shendale, Sarah Loving, Anita Milicic, and Andy Pollard for their helpful comments and suggestions on earlier draft versions of this entry.
See all interactive charts on vaccination ↓
Related topics
Smallpox
How has vaccination eradicated smallpox?
Disease eradication
Which diseases could be eradicated and how?
Child & infant mortality
What are children dying from and how can we prevent it?
Other research and writing on vaccination on Our World in Data:
- Our history is a battle against the microbes: we lost terribly before science, public health, and vaccines allowed us to protect ourselves
- How many people support vaccination across the world?
- How new vaccines can help with our antibiotic dependence
- Reduction of cases and deaths of vaccine-preventable diseases in the US
- Skepticism to vaccines and what to do about it
- Which countries have mandatory childhood vaccination policies?
Not every child who should be vaccinated is vaccinated
Global vaccine coverage
This chart shows the global vaccination coverage of one-year-olds with some of the most important vaccines recommended by the WHO. For many essential vaccines, coverage is now much higher than 80%. However, the rates of vaccination are still not sufficient.1
If you click the play button you see that the coverage for most vaccines has increased substantially over time.
The DTP vaccine (against diphtheria, tetanus, and pertussis) is often used as a key metric for global vaccination coverage because it involves three doses, and is a good indicator of access to routine immunization services.
In 2021, coverage of the third dose of DTP was 81%. This means that 81% of one-year-olds had received the third dose of the DTP vaccine and 19% had not.
In 2021, only 49% of one-year-olds globally received the rotavirus vaccine, which protects children from diarrheal diseases — one of the leading causes of child mortality. Similarly, the pneumococcal vaccine that protects children from pneumonia — the leading cause of child mortality — only reached 51% of one-year-olds.2

Number of one-year-olds who have received different vaccinations
See the data in our interactive visualization
Prosperity and vaccination coverage
Why do not all children in the world receive vaccinations?
The vaccine coverage against diphtheria, pertussis, and tetanus (DTP) is a good marker of the strength of a country’s immunization programs since several administrations are required.
This chart shows that poorer countries tend to be those with lower vaccination coverage for DTP. Similarly, countries in which a large share of the population is living in extreme poverty often — but not always — have lower immunization rates, as this related chart shows.
How vaccines work & herd immunity
Vaccines prime us to fight against infectious diseases. The basic mechanism by which vaccines work is simple: vaccines include a weakened or killed form of the pathogen, or just a part of the pathogen, which stimulates our immune response. This means that when we encounter the real pathogen later on, our immune system is better able to recognize it and protect against it.
When a person is immune to a disease, they can act as a barrier to slow down or prevent the spread of disease to other people. Populations that have more immunity are better able to contain the spread of the disease. This protects the rest of the population, especially those who cannot be vaccinated, such as very young infants and those who have immune conditions.
The "herd immunity threshold" refers to a level of immunity in the population above which the spread of disease slows down, or is unable to cause a lasting outbreak. This threshold depends on the context — it varies between different diseases and populations, and it can change over time.3
Progress made with vaccination
Since the first vaccine — the smallpox vaccine developed by Edward Jenner in 1796 — many more vaccines have been developed. As of 2023, effective vaccines are available against 33 human diseases.4
Smallpox and the origin of vaccination
Vaccination has a long history. An early form of vaccination was referred to as "variolation" or more broadly as "inoculation”. Practiced for a long time in Asia, this was an ancient technique of deliberate smallpox infection, in which dried smallpox scabs were blown up the nose, to infect the person with a milder form of the disease. By the 1700s, variolation had spread to Africa, India and the Ottoman Empire, followed by Britain and America, where the method of infection more frequently used a skin puncture.
Variolation could be effective but carried risks. If the pathogen wasn’t dried up or inactivated properly, then people who were variolated could contract the severe form of smallpox, which could be fatal, and could also spread the disease to others.
In 1796, the English physician Edward Jenner demonstrated another method of inoculation, in which he relied on cowpox. Cowpox is a similar disease to smallpox, and it had previously been observed that an infection with cowpox can protect against smallpox.
Jenner conducted an experiment using matter from a cowpox lesion to inoculate his gardener’s eight-year-old son James Phipps. Two months later Jenner exposed the boy to smallpox lesion matter and when Phipps did not develop smallpox, he concluded that he was protected against the disease. Jenner called the procedure "vaccination" after "vacca", the Latin word for cow, because of the origin of this first vaccination from the cowpox virus.
Following the findings of Jenner, the smallpox vaccine went through many iterations, with the newer vaccines produced by modern cell culture techniques (passing the virus through cell culture to make the vaccine safer).
By the middle of the 20th century, confidence grew that smallpox could be the first disease that humankind might be able to eradicate. In 1967, the WHO launched a global eradication of smallpox program. Mass vaccination of over 80% of populations was needed, but people who were nomadic or lived in politically unstable regions posed particular problems.
A number of innovations came in the development of the foot-powered injector, called the “ped-o-jet”, and the bifurcated needle, which was efficient and cheap.
To reach large sections of the population, the epidemiologist William Foege developed "Eradication Escalation (E2)" to contain smallpox outbreaks during October (the seasonal low point of smallpox transmission where prevention of just a few cases could stop a smallpox chain transmission).
Other obstacles in the program included forcibly vaccinating an Indian religious leader to convince his followers to be vaccinated, negotiation of ceasefires for vaccine transport in war-torn Nigeria, vaccinating in concentric rings around an outbreak, and cash bounties to reward the reporting of smallpox cases.
Finally, in 1977, the last case of naturally contracted smallpox was reported in Somalia — in a health worker called Ali Maow Maalin — and in 1980 the WHO announced that smallpox had been eradicated.
Read more on our page on smallpox:
Smallpox
Humanity eradicated this infectious disease globally. How was this possible?
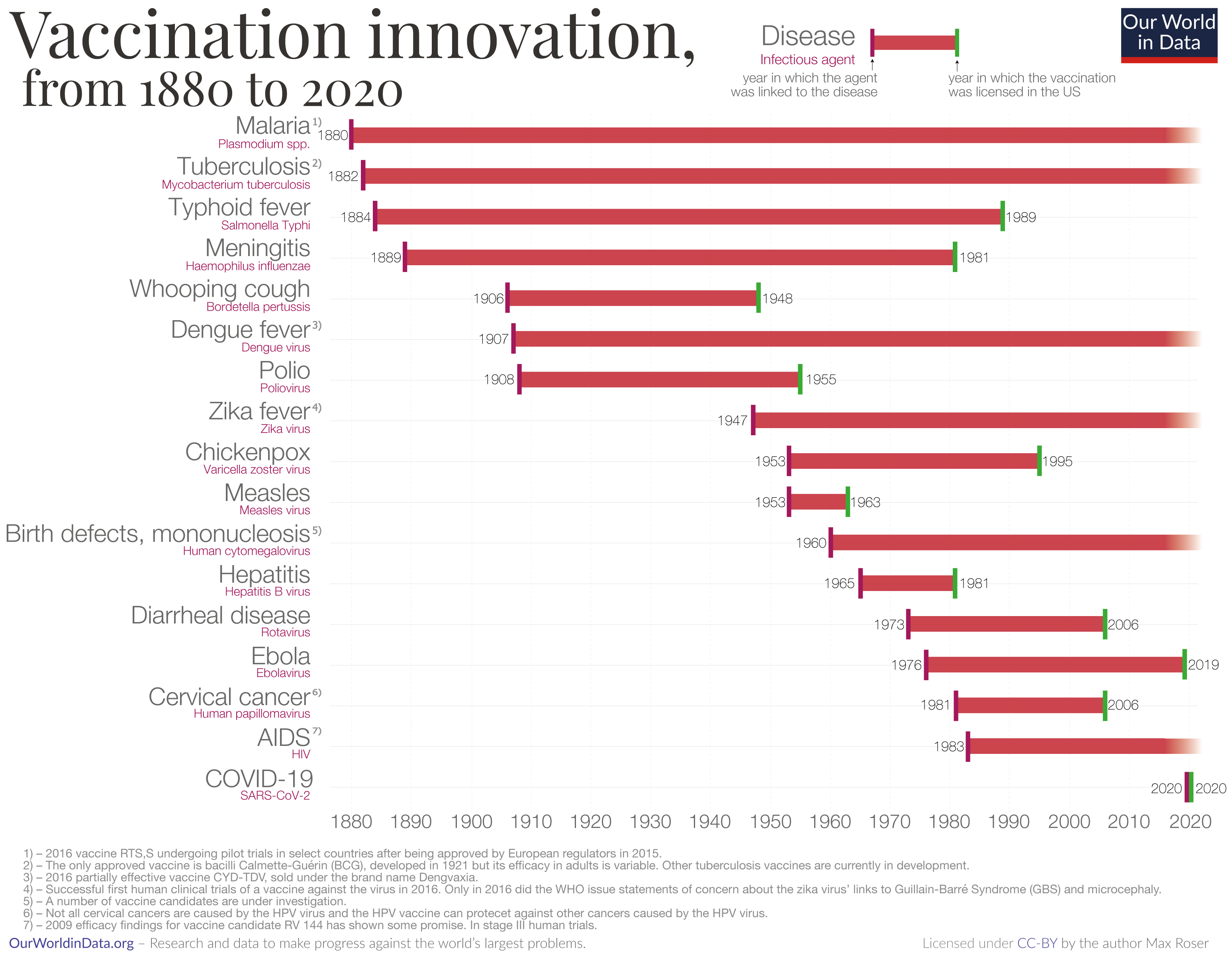
Vaccine innovation
The chart here shows a timeline of innovation in the development of vaccines as of 2020. Each bar begins in the year when the pathogenic agent was first linked to the disease, and the bar ends in the year when a vaccine against that pathogen was licensed in the United States.
For some diseases, there has been a relatively short period between when the pathogen was linked to the disease and when a vaccine was developed.
Before 2020, the quickest development was for measles. The measles virus was linked to the disease in 1953 and the vaccine was licensed in the U.S. in 1963.
In 2020, this record was broken when several vaccines were developed within just one year to fight the coronavirus pandemic.
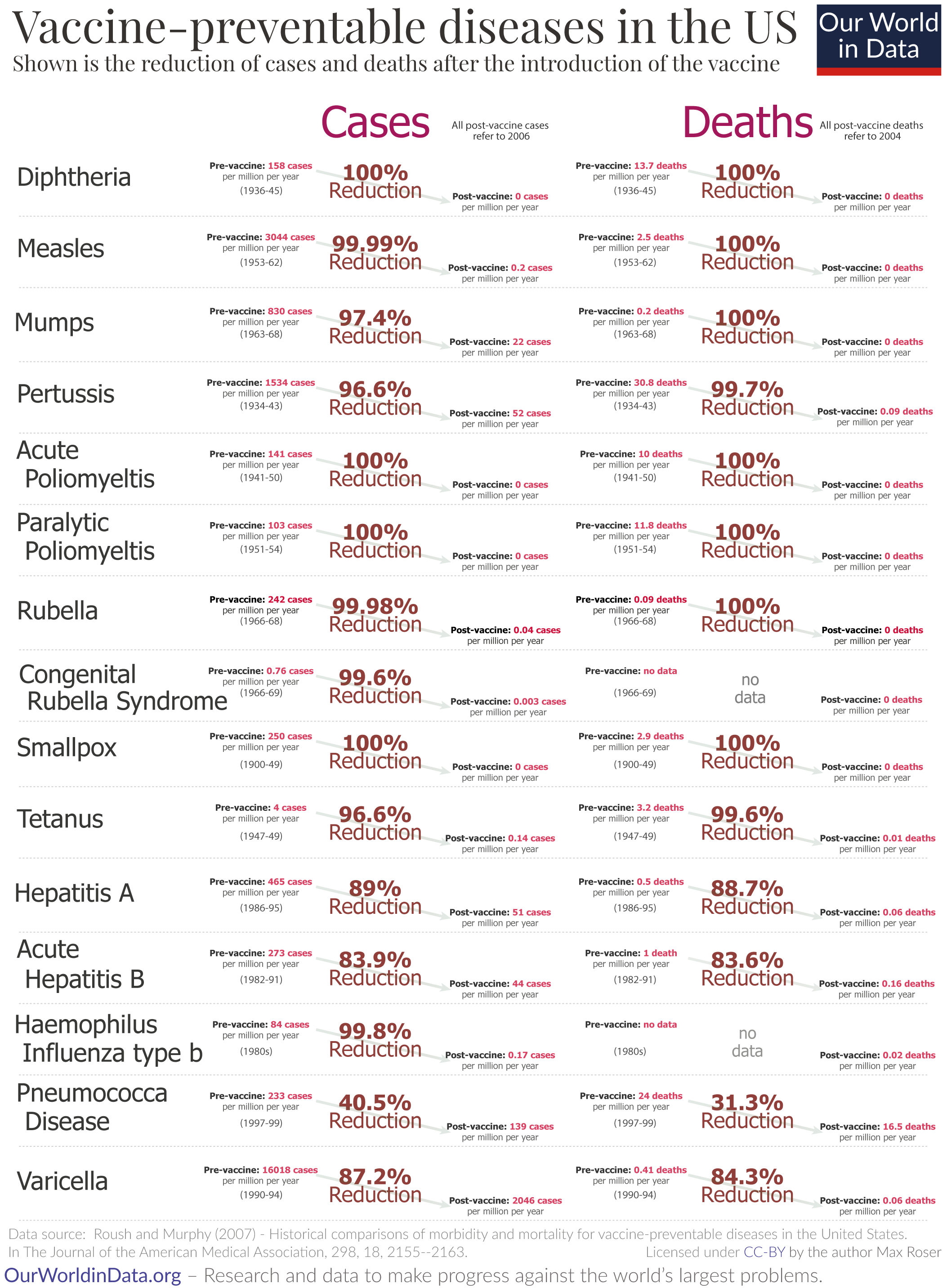
Progress against vaccine-preventable diseases in the US
The visualization here shows the reduction in cases and deaths from vaccine-preventable diseases in the United States after the introduction of each vaccine. This data was published by Roush and Murphy (2007).5
For several diseases, the US has achieved a 100% reduction of cases and deaths and for many other diseases, the reduction is often very substantial as well.
The development of the vaccine against measles and the history of measles in the US
The introduction of a vaccine was not the only reason for progress against these diseases, as the visualization shows.
The death rate of measles was falling in high-income countries such as the US before the vaccine was introduced in 1960 — this is best seen by switching from the linear to the logarithmic axis. Improved living conditions, nutrition, and medical advancements meant that contracting measles became less likely to be fatal.
But the rate of new cases of measles remained stable until the measles vaccine was introduced — as the chart shows.7
A chart showing the total number of cases and deaths can be seen here.
Global decline in vaccine-preventable diseases
The chart shows there has been a decline in the deaths caused by vaccine-preventable diseases, among children under five years old. This includes deaths caused by measles, tuberculosis, tetanus, meningitis, and other diseases.
But it also shows how much more needs to be done — even in recent years, millions of deaths have been caused by diseases that can be prevented by vaccines. In the following sections, we cover these diseases in more detail.
Public support and skepticism
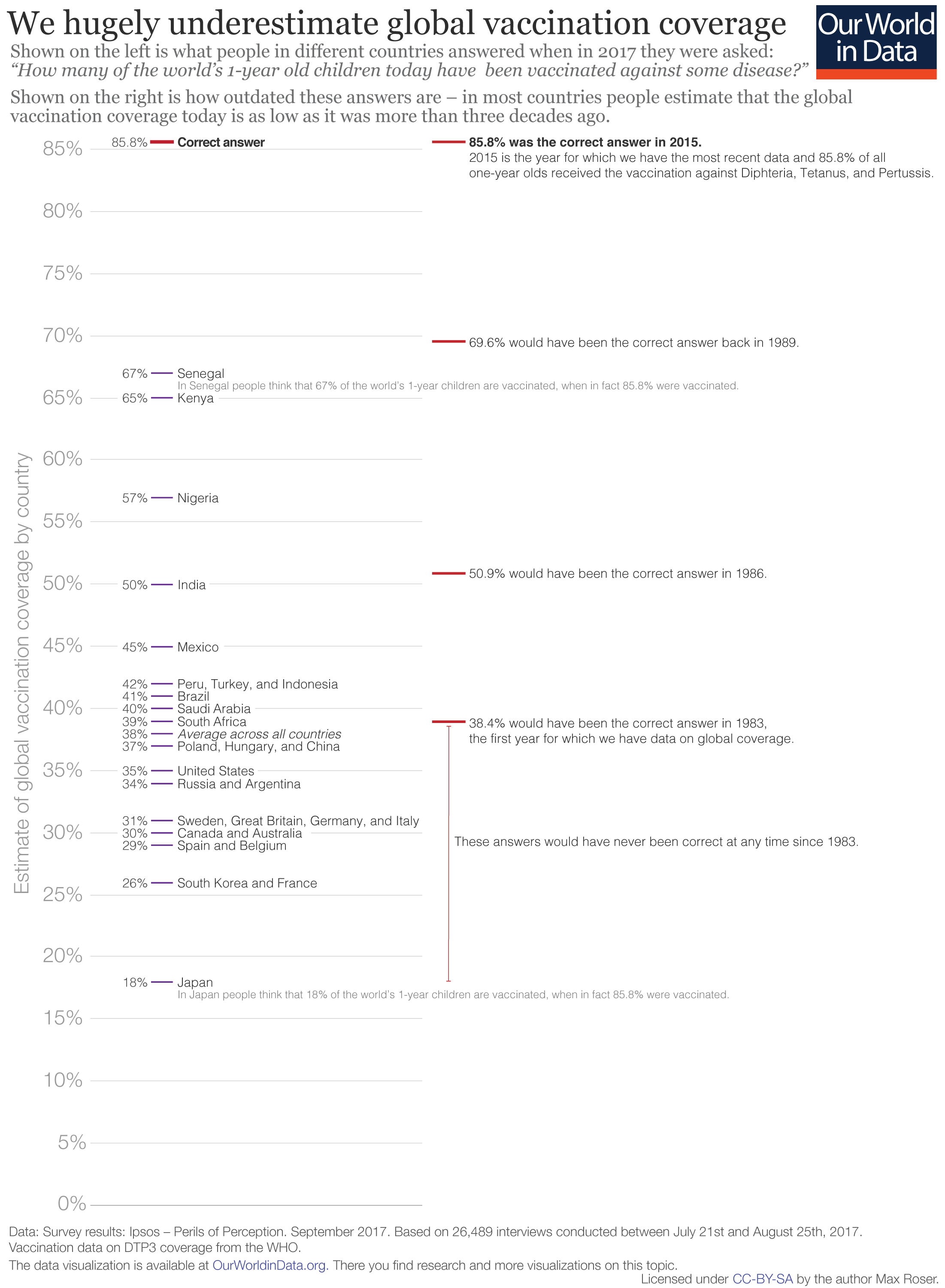
People do not know how well we do in global vaccination
Today vaccines protect millions of people around the world from infectious diseases. In this fight, we are much, much further ahead than most people realize.
People around the world have been asked the question: “How many of the world’s 1-year old children today have been vaccinated against [a particular] disease?” in large-scale surveys. For diphtheria, tetanus and pertussis, the correct answer was 86% in 2015. That’s the share who have been vaccinated with the third dose of the DTP vaccine.
But in all countries that were surveyed, people’s answers were much too pessimistic.
For example, Americans thought that only 35% of the world's children are vaccinated, while the true coverage was 50 percentage points higher.8 In Japan, people were even more pessimistic and thought that only 18% were vaccinated.
As is often the case in questions on global development, we again see that people in poorer countries have a more accurate view of the world: in Kenya and Senegal people thought that vaccines reached around two-thirds of all children in the world, but even these highest estimates were 20 percentage points too low.
The chart illustrates how outdated people's answers are. Most individuals think that the global vaccination coverage today is as low as it was in the 1980s or even earlier.
Read more in our articles:
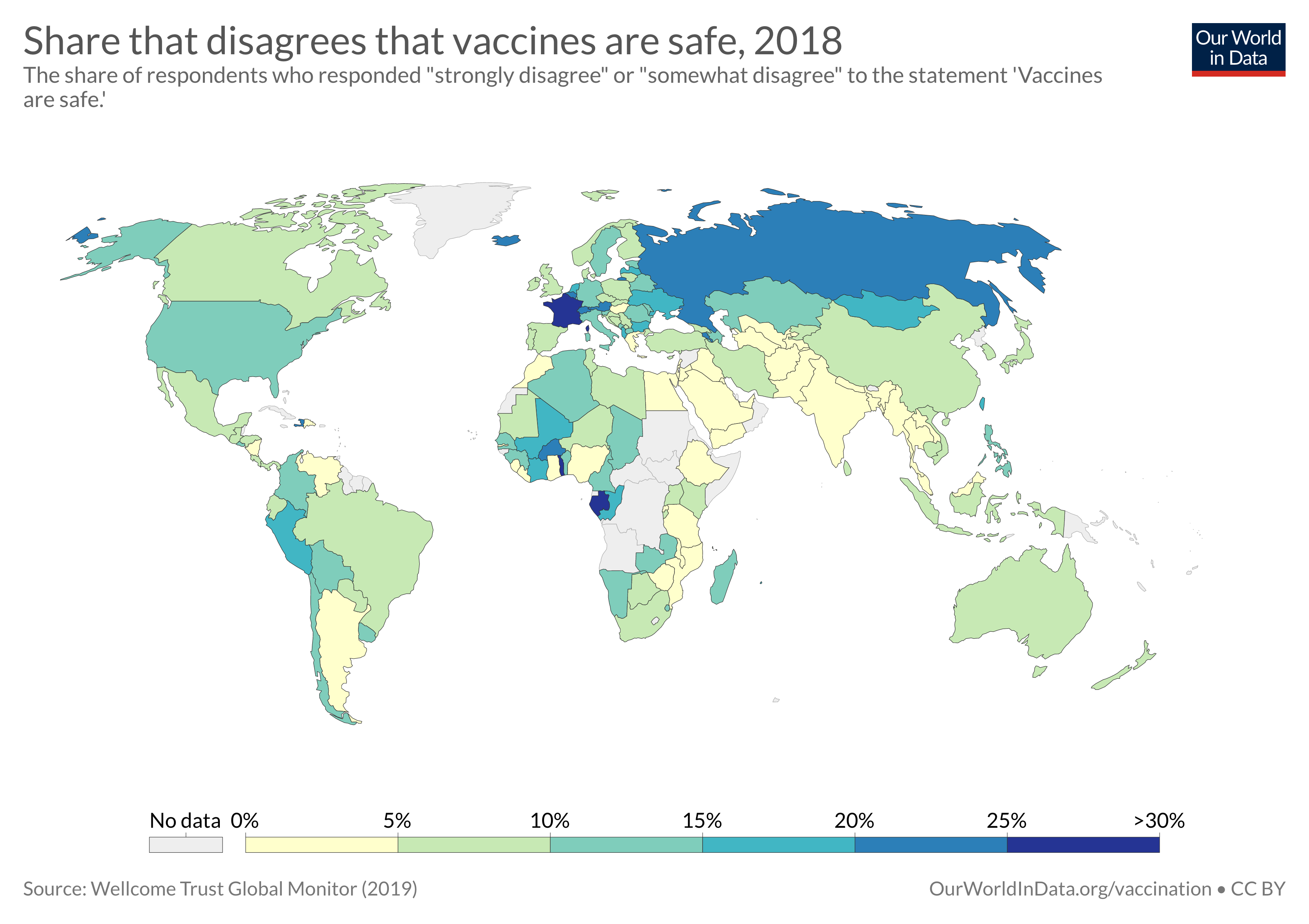
How many people support vaccination across the world?
Here we look at results from the largest global survey to date – the Wellcome Global Monitor – on attitudes to vaccination across the world.
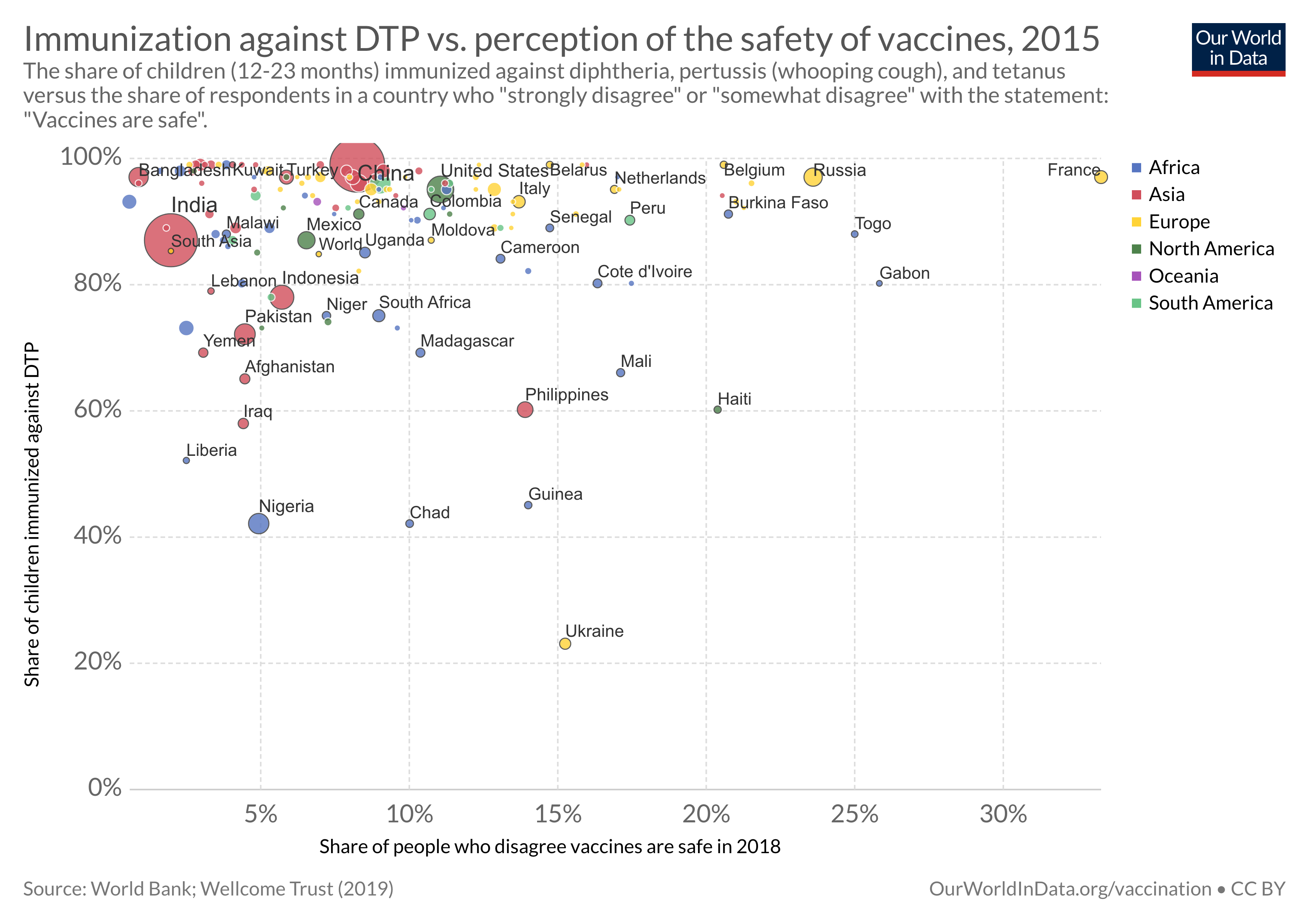
Skepticism to vaccines and what to do about it
What effect do public attitudes have on vaccine coverage rates, and what can we do about skepticism to vaccines?
Vaccine policy
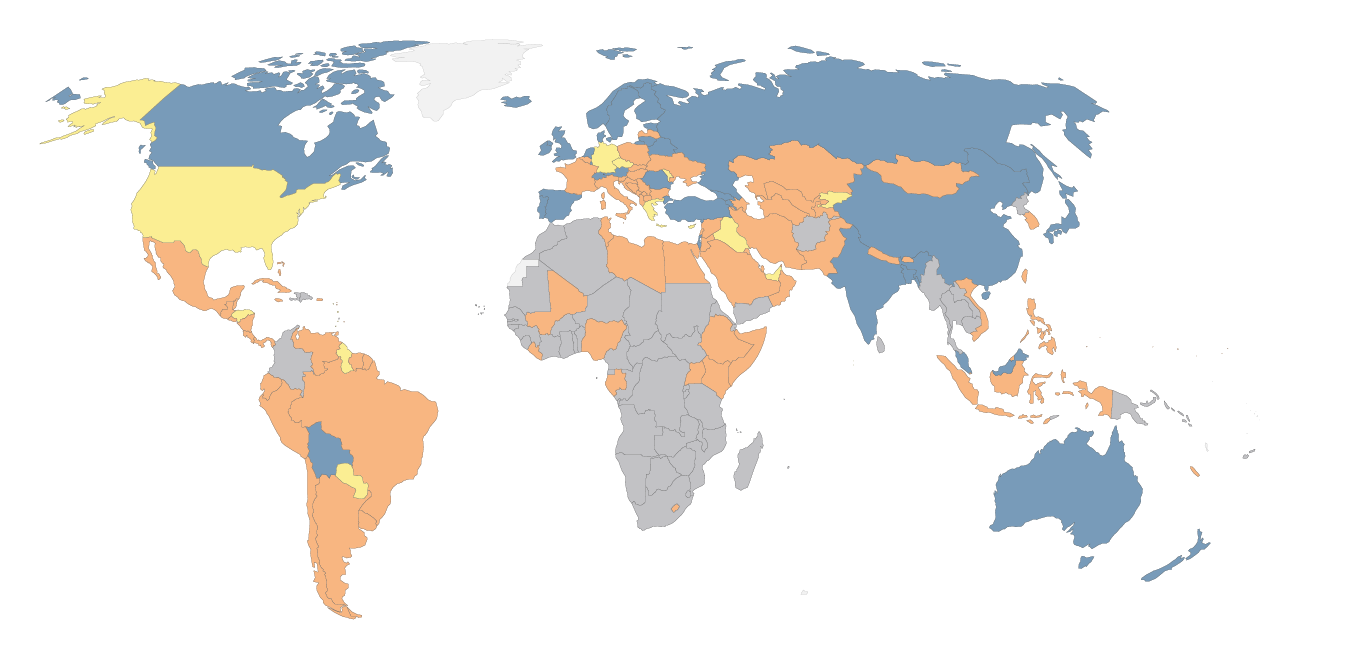
What determines if vaccinations are compulsory?
Countries vary in whether vaccination is compulsory, mandatory (required according to specific mandates), or voluntary.
Navin and Largent (2017) provide a helpful distinction between these policies. A compulsory policy is when refusing vaccination is illegal, while mandatory vaccination is when certain goods and services are limited for not vaccinating.10
Which policy is followed has depended much on historical legacy, which becomes clear when one considers some of the different regulations and their history around the world:
Compulsory vaccination: Many Eastern Bloc countries introduced compulsory vaccination during the communist era. Italy and France also had compulsory vaccination for three diseases, but increased this number to 11 in January 2018 in response to a drop in vaccination rates.
Mandatory vaccination: Some countries, such as the United States, have mandates for vaccination where a child is required to be vaccinated to enter state school or daycare.
An early case in the US paved the way for state jurisdiction to protect public health in light of personal liberty.11 In Jacobson v. Massachusetts (1905) the Supreme Court ruled that states have the authority to require vaccination against smallpox during a smallpox epidemic. Since then the US has had a history of school vaccination requirements. The increased number of children in public schools as a result of the compulsory school attendance law led to an increased risk of smallpox outbreaks, through close contact in large crowded classrooms.12
Similarly, in Australia, two policies penalize parents for not vaccinating their children. The "No jab no play" policy removed unvaccinated children from state-sponsored childcare. The 2016 "No jab no pay" policy removes state welfare by not providing the universal "Family Allowance" welfare payments for parents who are conscientious objectors of vaccination.
Read more in our article:
Which countries have mandatory childhood vaccination policies?
How do policies on childhood vaccinations vary across the world?
Voluntary vaccination: Some countries where vaccination is voluntary had early pushback against vaccination, such as the UK and the Netherlands. In 1853, a law was passed in England and Wales requiring universal vaccination against smallpox, but opposition from anti-vaccinationists led to laws being passed to allow for conscientious objection.13
Vaccination requirements for country entry: For countries in Africa and South America where yellow fever is endemic or where the mosquito vector is present a certificate of proof of vaccination is required. Only then will the country issue a visa upon entry to that country to prevent the importation of this disease (particularly if travelers come from, or have visited other yellow fever endemic areas).14
In past centuries (17th to 19th), yellow fever was transported to North America and Europe, causing large outbreaks that disrupted economies and development, and in some cases decimated populations. Throughout the 18th and 19th centuries, yellow fever was among the most feared diseases in the ports of the Old and New World. Saudi Arabia is the only country that requires additional vaccinations for meningococcal disease and polio for pilgrims visiting Mecca.
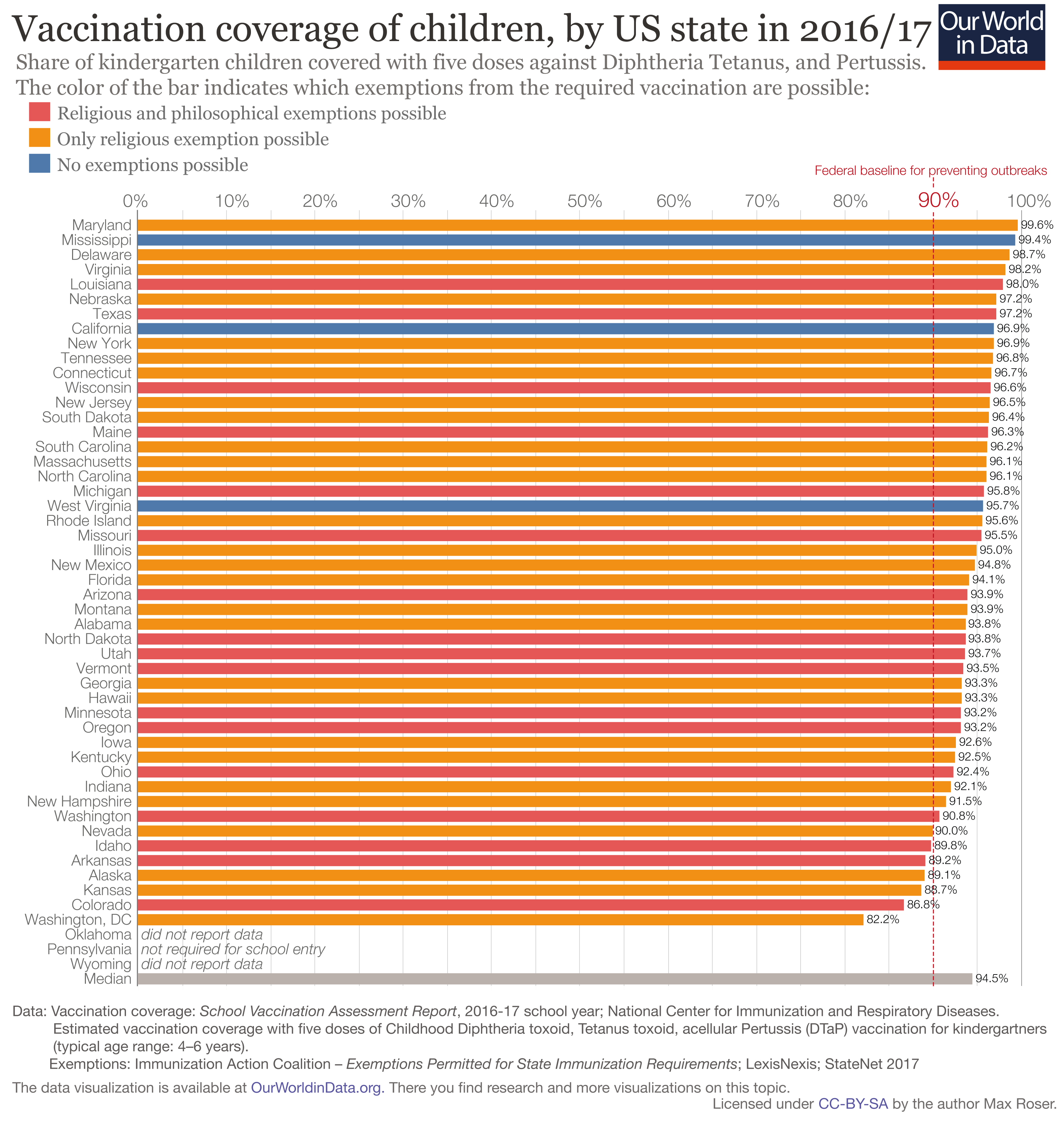
One country where we can see the effect of variation in vaccination policy is the US. In the US states decide what vaccine exemptions are permitted for children who receive education in schools or use daycare.
In individual states, exemptions are granted for medical reasons but many states also allow for philosophical, personal belief, or religious exemptions. Some states only allow for medical exemption.
The chart here shows vaccination coverage and what exemptions are allowed for each state. Fewer exemptions generally mean higher vaccine coverage.
Which countries include vaccines in their immunization schedules?
Several vaccines, including rubella, mumps, and rotavirus, are included in immunization schedules in many countries around the world. This means these vaccines are provided and recommended through routine services.
This doesn't necessarily tell us how many children receive these vaccines in each country. The vaccines may or may not be mandatory and their coverage rates may vary widely. Similarly, when countries do not have a vaccine in their schedule, this does not mean that the vaccine is completely unavailable in those countries, as it may be optional or available commercially.
In the map, you can see which countries include rubella vaccines in their national immunization schedules. Rubella vaccines became available for the first time in 1969, starting in the United States, where it was developed.16 It was included in the schedules of the United States and most European countries as early as 1994 (the first year of this dataset). Over time, more countries included it in their schedule.
But this took many years for some countries: for example, it took until 2018 for it to be included in countries such as Uganda and Congo.
As of 2021, some countries, such as Nigeria and South Africa, still do not include it in their schedules.17
In the links below, you can see these charts for other vaccines.

Which countries include Haemophilus influenzae B (Hib) vaccines in their vaccination schedules?
See the data in our interactive visualization

Which countries include hepatitis B vaccines in their vaccination schedules?
See the data in our interactive visualization

Which countries include hepatitis B birth dose vaccines in their vaccination schedules?
See the data in our interactive visualization

Which countries include human papillomavirus (HPV) vaccines in their vaccination schedules?
See the data in our interactive visualization

Which countries include inactivated poliovirus (IPV) vaccines in their vaccination schedules?
See the data in our interactive visualization

Which countries include MCV2 vaccines in their vaccination schedules?
See the data in our interactive visualization

Which countries include mumps vaccines in their vaccination schedules?
See the data in our interactive visualization

Which countries include pneumococcal conjugate vaccines (PCV) in their vaccination schedules?
See the data in our interactive visualization

Which countries include rotavirus vaccines in their vaccination schedules?
See the data in our interactive visualization
Coverage, Impact, and Potential
Diseases preventable through vaccination
The chart shows the number of global deaths caused by some of the most common and serious vaccine-preventable diseases.
By selecting "change country" it is possible to see this change for any country in the world and extending the timeline will let you see the change in deaths over time.
There are more diseases for which vaccines are available now and even more are under development currently. The WHO publishes list of 26 diseases for which vaccines are available — including Japanese encephalitis, pneumococcal disease, varicella/chicken pox, HPV, Hepatitis A, and rotavirus.
Diphtheria, Tetanus, and Pertussis vaccine
Diphtheria, tetanus, and pertussis are all bacterial diseases, and a combination vaccine (called the DTP vaccine) is commonly used to protect against all three diseases.
- Diphtheria is a serious bacterial infection that affects the throat and nose. It can lead to breathing difficulties, heart failure, and paralysis.
- Tetanus is a disease caused by the bacteria Clostridium tetani. It can be caught from dirt that enters wounds, which especially affects mothers giving birth and newborns. The bacteria release a toxin that prevents the normal functioning of nerves, and can eventually lead to paralysis, difficulty breathing, and death.
- Pertussis, also known as whooping cough, is a highly contagious respiratory infection that is known for severe coughing fits followed by a "whooping" sound.
The chart shows the progress over time of DTP3 immunization coverage of children around the world. By clicking on any country you can see the change in that country over time.
One region that stands out is South-East Asia. While 82% of one-year-olds in the region were vaccinated in 2021, that figure had been just 7% in 1980.
Measles vaccine
Measles is a highly contagious virus spread through airborne particles. It causes serious disease, especially among children.
The world map shows the share of children vaccinated with the first dose of measles vaccine.
You can switch to the "chart" view to see the global coverage against vaccines. The measles vaccine was developed in 1963. In 1980, less than 20% of children were vaccinated globally. By 2021, that figure was over 80%.
Second dose of measles vaccine provides greater protection
Two doses of the measles vaccine are needed for a higher level of protection.18
The map here shows the coverage of the second dose (MCV2) of the measles vaccine.19
Global decline of measles
The second visualization shows the discussed increase of the global vaccination coverage of one-year-olds and the simultaneous decline of reported cases of the disease; from close to 1,000 cases per million people globally to 28 cases per million. This represents a 33-fold reduction.
For country by country change over time see this visualization.
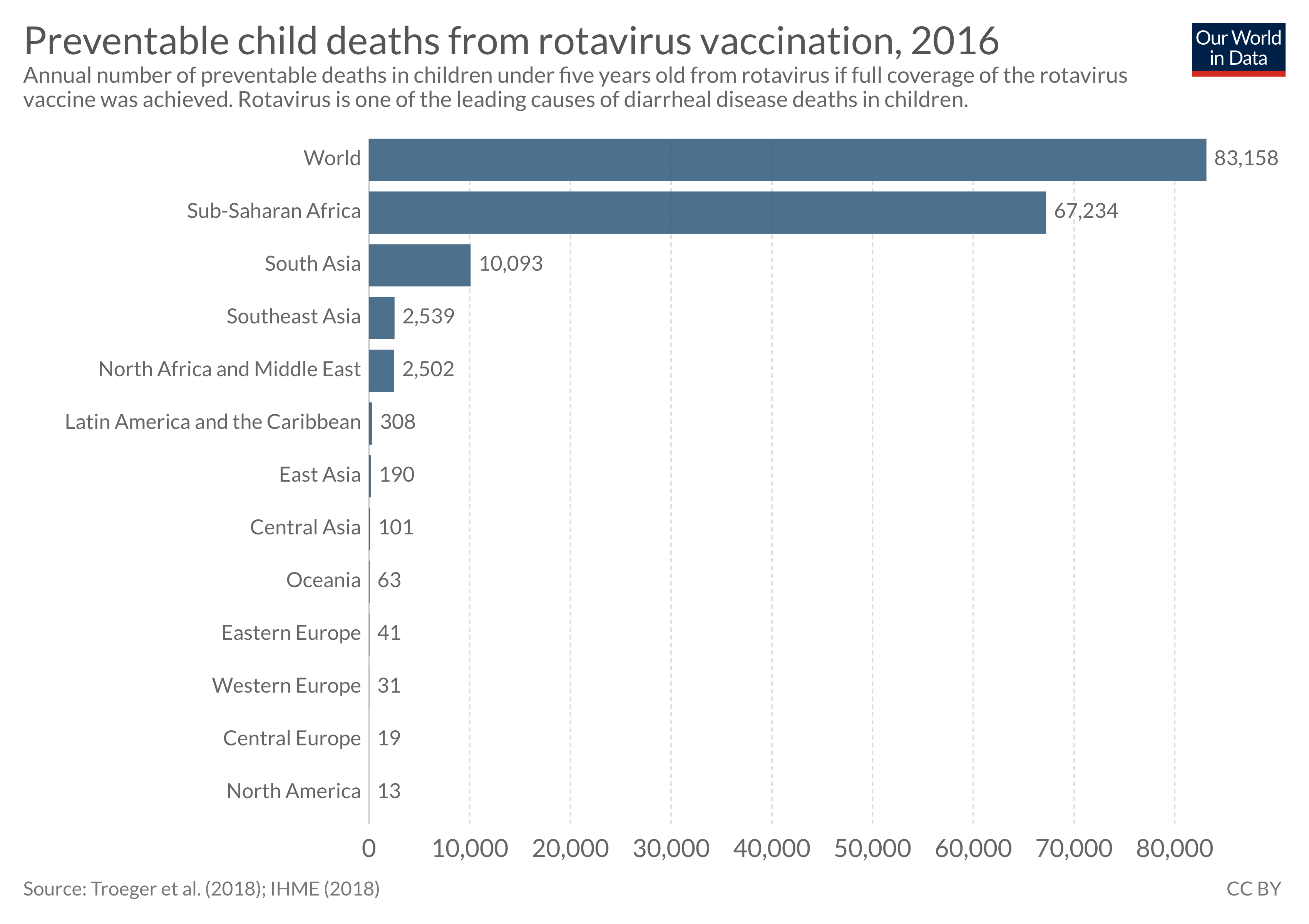
Rotavirus vaccines
Rotavirus is the most common cause of diarrheal deaths in children globally.
Although rotavirus vaccines were first introduced in the United States in 2006, the death rate remains high because children in many countries do not receive vaccinations.
The efficacy of rotavirus vaccines has also been lower in countries with higher death rates.20
In the chart, you can see the share of one-year-olds who were vaccinated against rotavirus.
By increasing vaccination rates, more children can be protected against the virus, and a major cause of diarrheal deaths can be prevented.21
Read more about the rotavirus vaccine:
Rotavirus vaccine - an effective tool that prevents children dying from diarrhea
Rotavirus is the leading cause of diarrheal deaths in children. There is, however, an effective tool against it: the rotavirus vaccine.
Pneumococcal vaccines
There are a number of ways we could reduce the number of children dying from pneumonia, including eliminating the major risk factors such as undernutrition and air pollution, and providing better access to treatment.
But we also have another highly effective intervention: a vaccine against the major pathogen responsible for pneumonia in children, Streptococcus pneumoniae.22
Read more on our page on pneumonia:
Pneumonia
Pneumonia is the leading cause of death for children younger than 5 years.
Hepatitis B vaccine
The chart here shows the coverage for Hepatitis B vaccination.
Hepatitis B (HepB) is a highly contagious viral infection that attacks the liver and is transmitted through contact with the blood or other body fluids of an infected person. It can cause chronic liver disease and death.
The WHO recommends that all infants should receive their first dose of vaccine as soon as possible after birth, preferably within 24 hours.
Haemophilus influenzae type b vaccine
Haemophilus influenzae type b (Hib) is a bacterial infection that causes meningitis and pneumonia transmitted through the respiratory tract from infected to susceptible individuals. The chart here shows the coverage for Hib vaccination.
Polio vaccine
The chart here shows the coverage of the polio vaccine.
Polio is a highly infectious viral disease spread through contaminated food and water. In a fraction of people who are infected, it causes paralysis of the muscles, which can lead to death.
There are different types of vaccines against polio, including the oral poliovirus vaccines (OPV) and the inactivated poliovirus vaccines (IPV). The chart below shows the share of one-year-olds who have received the third dose of a polio vaccine.
Read more on our page on polio:
Polio
The world has made great progress against polio and two out of three types of wild poliovirus have been eradicated. This page presents global data and research on polio and the remaining challenges in eradicating the disease.
Tuberculosis vaccine (BCG)
The chart here shows the coverage of the BCG vaccine, which protects against tuberculosis.
The BCG vaccine is one of the oldest and among the most widely used vaccines in the world.23 It is based on a mild strain of Mycobacterium bovis, a bacterium that is closely related to Mycobacterium tuberculosis — the pathogen that causes TB.
The BCG vaccine became used in the 1920s in Belgium and France in small trials and after the Second World War its use was expanded to vaccinate children across Europe. In the 1950s, the WHO started recommending the use of the BCG vaccine globally.
BCG is effective at protecting children and adolescents from severe forms of TB and meningitis.24 25 However, studies have shown that the length of protection provided by the vaccine varies greatly depending on the populations studied.26 27 The reason for such variability is not clear, but factors such as different vaccine seed strains used for immunization and pre-existing immunity in people already exposed to other mycobacteria strains may be important.
Notably, the BCG vaccine protects against severe disease — but it does not protect people from getting infected with M. tuberculosis bacterium in the first place, and doesn’t prevent activation of latent TB if a person has already been infected. Therefore, the vaccine has limited effect on the prevention of M. tuberculosis spread in a population.28
Yellow fever vaccine
The chart here shows the coverage of the yellow fever vaccine.
Yellow fever (YF) is a viral disease transmitted by infected mosquitoes. The charts show the coverage of yellow fever across countries. As you can see, it is mainly used in countries in South America and West Africa.29
Endnotes
Terminology: vaccination and immunization
There is a technical difference between vaccination and immunization, as the National Health Service (NHS) explains: “Vaccination means having a vaccine — that is actually getting the injection, or nasal spray or oral vaccine. Immunization means both receiving a vaccine and then becoming immune to a disease”. The distinction is made because in a very small number of those who are vaccinated the vaccination will not "take" and therefore that vaccinated person will not be immunized (i.e. will not be immune to the disease). However, as this refers to a very small number of people both terms are often used interchangeably across the academic literature and in media reporting and we follow this convention in this entry.
This and other numbers in this entry are based on estimates by the World Health Organisation. The coverage estimates are calculated by dividing the total number of vaccinations given by the number of children in the target population. Target population size is usually based on census population projections.
This means that there may be children in the target population who should be exempt from vaccination for medical reasons, such as severe immunodeficiencies to allergies to vaccine components.
Notably, such cases are very rare and would have little effect on global coverage numbers. For example, a study from 2003 identified severe allergic reactions in only 0.000063% of all vaccinations, which is 0.63 cases per million vaccinations. In addition, vaccines are always being improved with fewer ingredients that may cause allergic reactions.
Vaccination of children with immunodeficiencies generally needs to be assessed by a specialist. Especially, for vaccines that are based on live pathogens. For example, WHO recommends vaccinating HIV-positive children with the measles vaccine if the child's HIV infection is asymptomatic or not severe. Similarly, children with severe immunodeficiency syndrome (SCID), a genetic disorder that causes defects in the immune system, are safely vaccinated with many vaccines before SCID is even diagnosed, but it's recommended not to vaccinate them with live vaccines.
One of the reasons it is important to increase vaccination rates is children and adults who cannot be vaccinated for medical reasons would still be protected from diseases through herd immunity.
See Oxford's Vaccine Knowledge Project for an explanation here: http://vk.ovg.ox.ac.uk/herd-immunity.
Smallpox, Rabies, Tetanus, Cholera, Typhoid, Diphtheria, Pertussis, Tuberculosis, Yellow fever, Anthrax, Influenza, Japanese encephalitis, Polio, Measles, Mumps, Rubella, Meningitis, Tick-borne encephalitis, Pneumococcal disease, Hepatitis B, Haemophilus influenzae b, Varicella, Hepatitis A, Human papillomavirus, Rotavirus, Zoster, Dengue, Ebola Zaire, Mpox, Covid-19, Malaria, Chikungunya, Respiratory syncytial virus.
See https://en.wikipedia.org/wiki/Vaccine-preventable_diseases and https://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/
Roush and Murphy (2007) — Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. In the Journal of the American Medical Association, 298, 18, 2155–2163. here
These data are taken from the research paper Roush and Murphy (2007) — Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. In the Journal of the American Medical Association, 298, 18, 2155–2163 here.
The vaccines against the diseases up till "Tetanus" were vaccines licensed or recommended before 1980. The vaccines against the last 5 diseases were only licensed or recommended between 1980 and 2005.
See also "Graphical proof that vaccines work (with sources)" in Medium online here.
To account for such long-term changes, Roush and Murphy (2007) report data from the period shortly before the introduction of the respective vaccine. here
This survey result is in line with the finding of the Gapminder Ignorance Project, which studied Americans' perception of global vaccination efforts. Just as in the Ipsos Mori survey, the answers that most Americans gave were far off from the truth.
More information on the Gapminder "Ignorance Test" can be found here. The results for the US are here on Gapminder's site.
The survey results are from Chris Jackson (2017) — Global Perceptions of Development Progress: "Perils of Perceptions’ Research", published by Ipsos MORI, 18 September 2017. Online here.
Navin M. Largent, improving non-medical exemption vaccine policies: three case studies. Public Health Ethics. 2017; 10: 225–234. Available here
Stern, M., Alexandra. (2010). Better Off in School: School Medical Inspection as a Public Health Strategy During the 1918-1919 Influenza Pandemic in the United States
Amin, A.N.E., Parra, M.T., Kim-Farley, R. et al. (2012) — Ethical Issues Concerning Vaccination Requirements. In Public Health Reviews (2012) 34: 14. https://doi.org/10.1007/BF03391666. Online here: https://link.springer.com/article/10.1007/BF03391666
The data source for vaccination coverage: School Vaccination Assessment Report, 2016-17 school year.
Estimated vaccination coverage with 5 doses of Childhood Diphtheria toxoid, Tetanus toxoid, acellular Pertussis (DTaP) vaccination for kindergartners (typical age range is 4–6 years).
The data source for exemptions is: Immunization Action Coalition, "Exemptions Permitted for State Immunization Requirements," 2017; LexisNexis; StateNet 2017
Regarding the school vaccination coverage and exemption methods the source notes: "Each school year, school nurses, other school personnel, or health department personnel check the vaccination and exemption status of kindergartners enrolled in public and private schools as required by state law or regulation. State and local immunization programs measure vaccination coverage among children entering kindergarten annually. This may be done for every student or for a sample of students.
State and local areas set the vaccination requirements. Immunization information systems (IISs) may be used as one source of data for school vaccination assessment. The school-level data are reported to the health department. The aggregate data are reported to CDC for public and private schools. Data for home-schooled students are not routinely reported to CDC."
The types of permitted exemptions vary by state. For specific details refer to School Vaccination Requirements and Exemptions.
Lanziera, T., Haber, P., Icenogle, J. P., & Patel, M. (n.d.). Rubella. In Epidemiology and Prevention of Vaccine-Preventable Diseases. Communication and Education Branch, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/pubs/pinkbook/rubella.html
World Health Organization. (2021). New and underutilized vaccines introduction. https://immunizationdata.who.int/pages/indicators-by-category/new_and_under_utilized_vaccines_introduction.html
Gaston De Serres, Jill Sciberras, Monika Naus, Nicole Boulianne, Bernard Duval, and Louis Rochette (1999) — Protection after Two Doses of Measles Vaccine Is Independent of Interval between Doses. In The Journal of Infectious Diseases, Volume 180, Issue 1, 1 July 1999, Pages 187–190, https://doi.org/10.1086/314847 Online here: https://academic.oup.com/jid/article/180/1/187/990623.
For guidelines on recommendations for the second dose of measles vaccine see here https://www.who.int/immunization/sage/meetings/2016/october/Session6-MCV2-Introduction-criteria.pdf
The effectiveness of rotavirus vaccines has been around 86% among children under 12 months in countries with low rotavirus mortality, and 63 or 66% in countries with high rotavirus mortality.
Burnett, E., Parashar, U. D., & Tate, J. E. (2020). Real-world effectiveness of rotavirus vaccines, 2006–19: A literature review and meta-analysis. The Lancet Global Health, 8(9), e1195–e1202. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(20)30262-X/fulltext
The reasons for a lower efficacy in poorer countries are unknown but may result from many factors. For example, other oral vaccines, including vaccines against polio and cholera, have also shown lower efficacies in poorer countries. This may be because children have co-infections with other enteric viruses, which reduce their gut immune response to the vaccines. Other potential factors include higher exposure to the virus and variations in gut microbiomes, blood groups, and immune antigens.
Burke, R. M., Tate, J. E., Kirkwood, C. D., Steele, A. D., & Parashar, U. D. (2019). Current and new rotavirus vaccines: Current Opinion in Infectious Diseases, 32(5), 435–444. https://doi.org/10.1097/QCO.0000000000000572
Burnett, E., Parashar, U., & Tate, J. (2018). Rotavirus Vaccines: Effectiveness, Safety, and Future Directions. Pediatric Drugs, 20(3), 223–233. https://doi.org/10.1007/s40272-018-0283-3
Kirkwood, C. D., Ma, L.-F., Carey, M. E., & Steele, A. D. (2019). The rotavirus vaccine development pipeline. Vaccine, 37(50), 7328–7335. https://doi.org/10.1016/j.vaccine.2017.03.076
Troeger, C., Khalil, I. A., Rao, P. C., Cao, S., Blacker, B. F., Ahmed, T., Armah, G., Bines, J. E., Brewer, T. G., Colombara, D. V., Kang, G., Kirkpatrick, B. D., Kirkwood, C. D., Mwenda, J. M., Parashar, U. D., Petri, W. A., Riddle, M. S., Steele, A. D., Thompson, R. L., … Reiner, R. C. (2018). Rotavirus Vaccination and the Global Burden of Rotavirus Diarrhea Among Children Younger Than 5 Years. JAMA Pediatrics, 172(10), 958. https://doi.org/10.1001/jamapediatrics.2018.1960
The authors estimate that the rotavirus averted around 28,000 deaths in children under five in 2016. They also estimate that an additional 83,200 deaths in this age group could have been averted if full vaccine coverage had been achieved that year.
Troeger, C., Blacker, B., Khalil, I. A., Rao, P. C., Cao, J., Zimsen, S. R., ... & Adetifa, I. M. O. (2018). Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet Infectious Diseases, 18(11), 1191-1210.
Kendig, E. L., Wilmott, R. W., & Chernick, V. (2012). Kendig and Chernick's disorders of the respiratory tract in children. 9th ed. Elsevier Health Sciences.
Rodrigues, L. C., Mangtani, P., & Abubakar, I. (2011). How does the level of BCG vaccine protection against tuberculosis fall over time?. Bmj, 343, d5974.
Rodrigues, L. C., Diwan, V. K., & Wheeler, J. G. (1993). Protective effect of BCG against tuberculous meningitis and miliary tuberculosis: a meta-analysis. International journal of epidemiology, 22(6), 1154-1158.
Sterne, J. A. C., Rodrigues, L. C., & Guedes, I. N. (1998). Does the efficacy of BCG decline with time since vaccination?.The international journal of tuberculosis and lung disease, 2(3), 200-207.
Aronson, N. E., Santosham, M., Comstock, G. W., Howard, R. S., Moulton, L. H., Rhoades, E. R., & Harrison, L. H. (2004). Long-term efficacy of BCG vaccine in American Indians and Alaska Natives: a 60-year follow-up study. Jama, 291(17), 2086-2091.
WHO BCG vaccine fact sheet: https://www.who.int/biologicals/areas/vaccines/bcg/en/
WHO Immunization Fact Sheet: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage
Cite this work
Our articles and data visualizations rely on work from many different people and organizations. When citing this topic page, please also cite the underlying data sources. This topic page can be cited as:
Samantha Vanderslott, Saloni Dattani, Fiona Spooner and Max Roser (2022) - “Vaccination” Published online at OurWorldInData.org. Retrieved from: 'https://ourworldindata.org/vaccination' [Online Resource]BibTeX citation
@article{owid-vaccination,
author = {Samantha Vanderslott and Saloni Dattani and Fiona Spooner and Max Roser},
title = {Vaccination},
journal = {Our World in Data},
year = {2022},
note = {https://ourworldindata.org/vaccination}
}Reuse this work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
All of our charts can be embedded in any site.