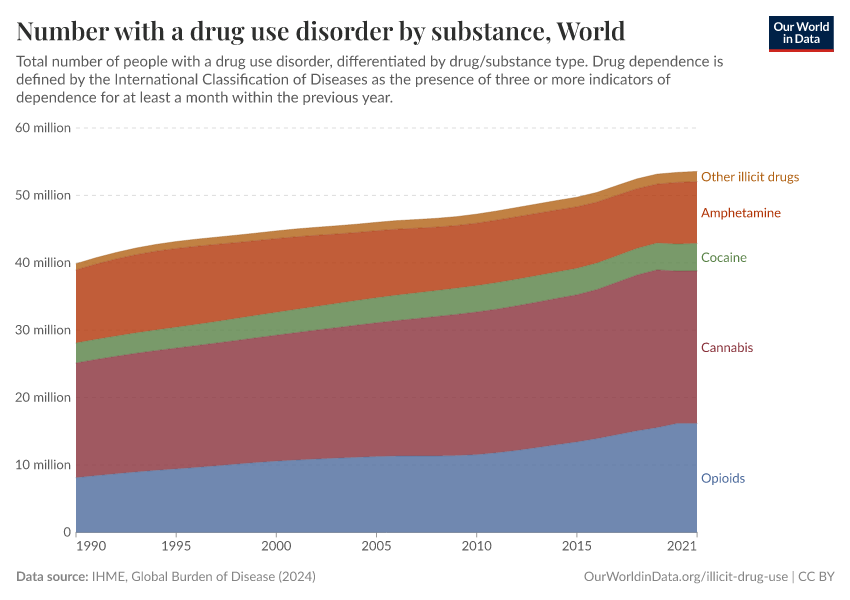
Opioids, Cocaine, Cannabis, and Other Illicit Drugs
How common is the use and addiction to opioids, cocaine, amphetamines and cannabis? What is the impact?
Illicit drugs are drugs that have been prohibited under international drug control treaties.1
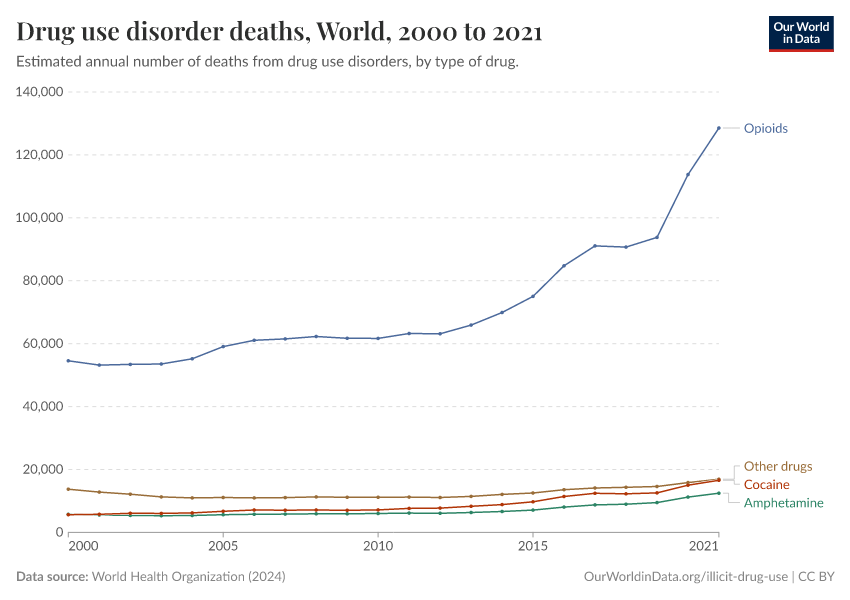
International statistics typically focus on four different groups of illicit drugs: opioids, cocaine, cannabis, and amphetamines. However, a range of other illicit drugs is included in international drug control treaties, including plant-based drugs and synthetic hallucinogens. The UNODC's publication "Terminology and Information on Drugs"2 contains a comprehensive list of illicit drugs.
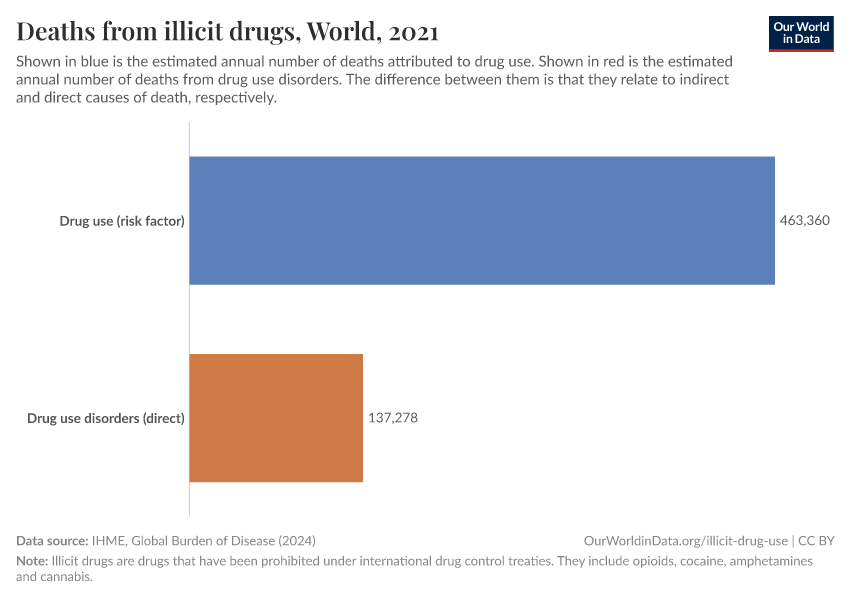
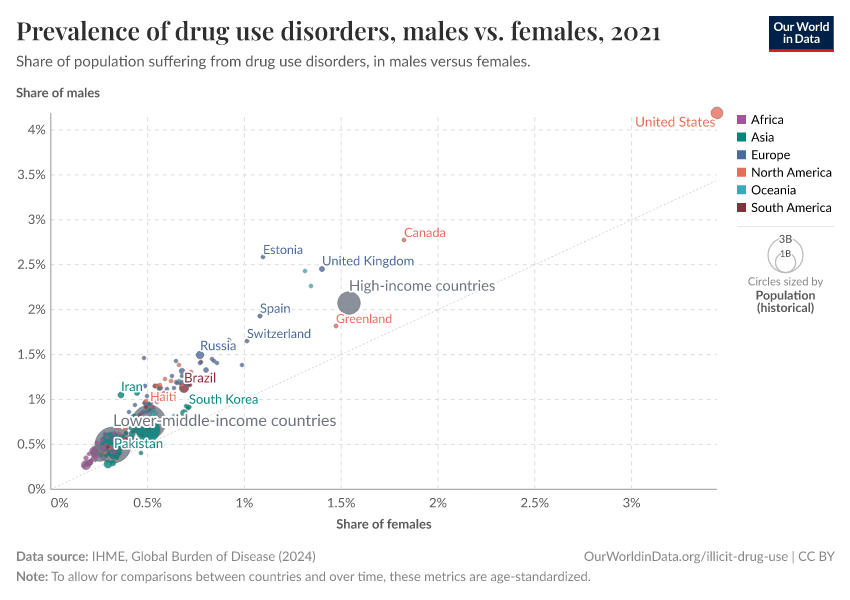
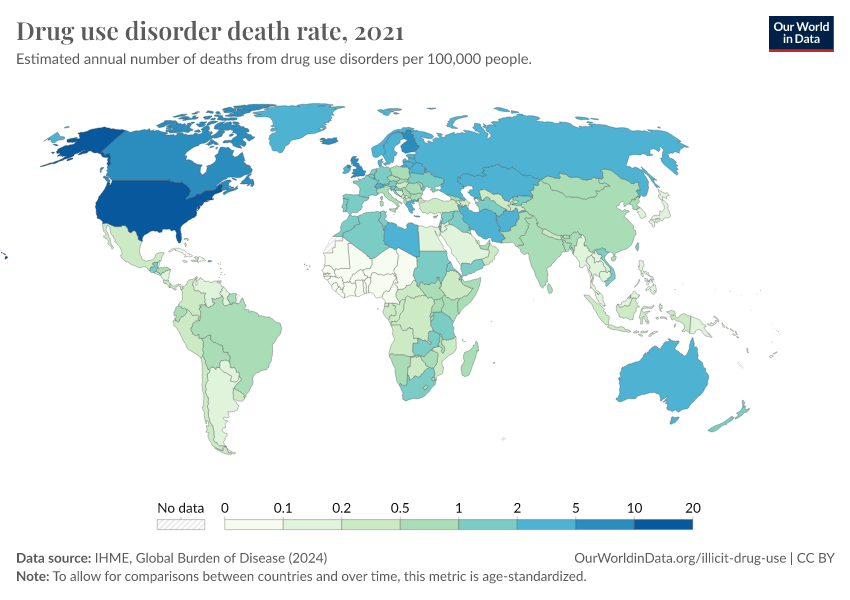
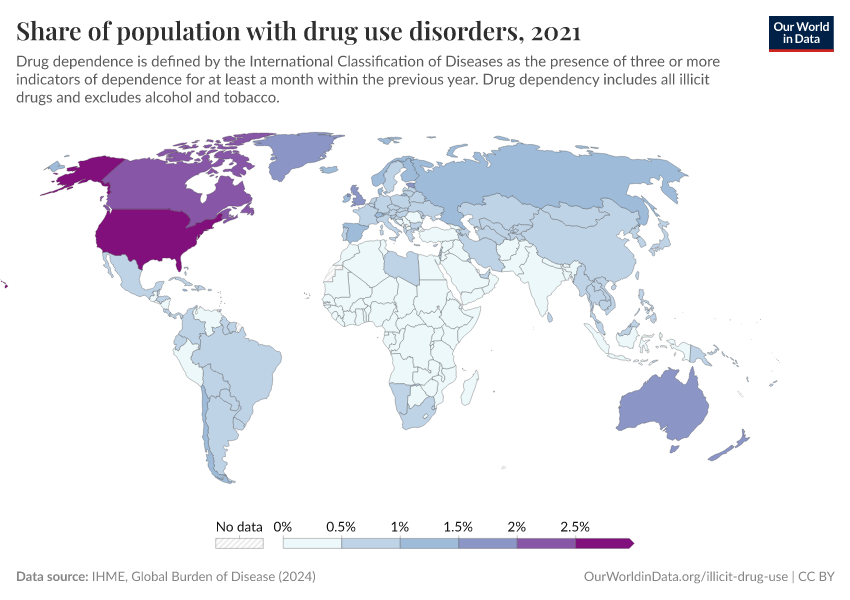
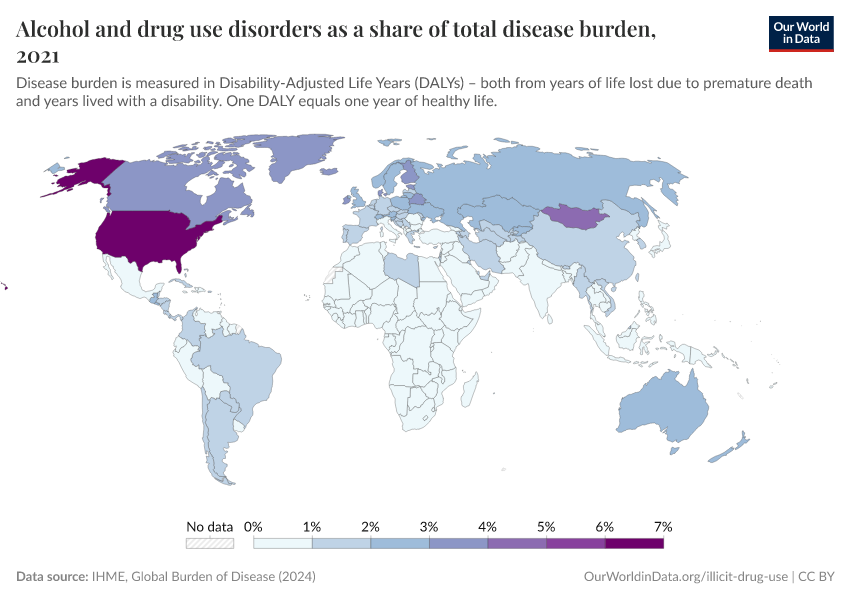
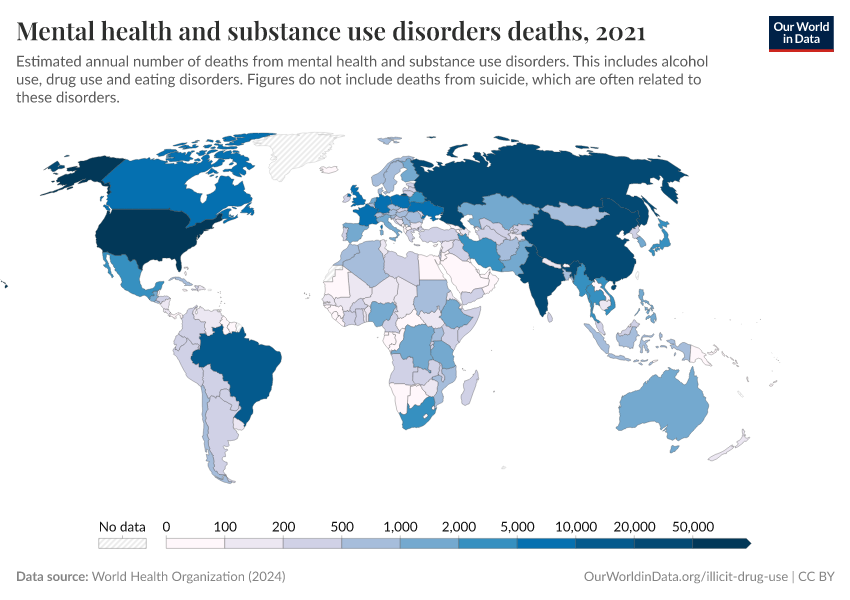
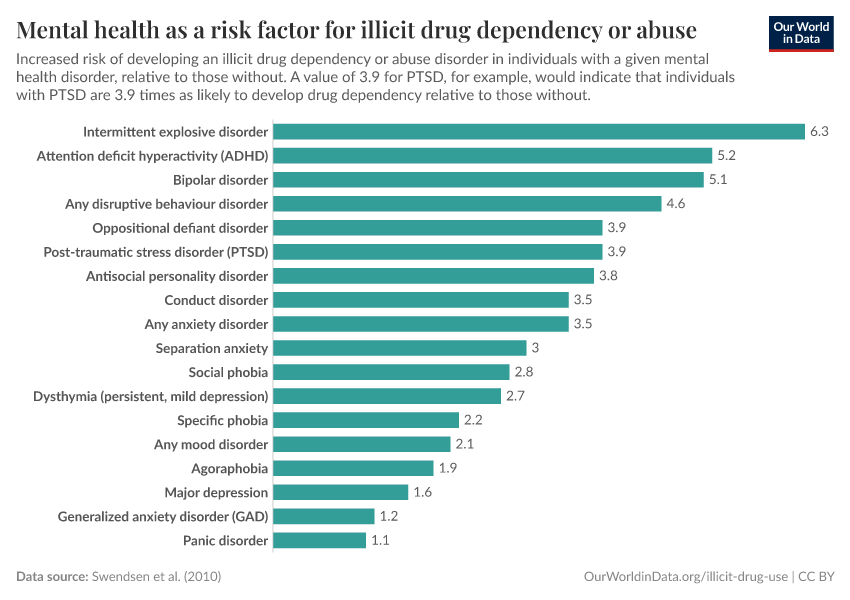
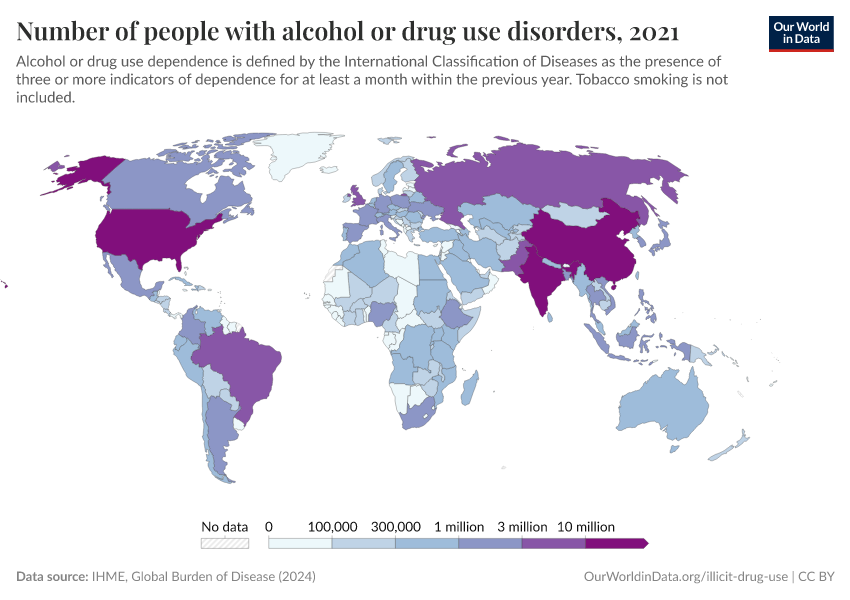
Excess consumption or dependency on illicit drugs can impact overall health, mental well-being, and in many cases, the well-being of others. Not all illicit drugs have similar impacts on health and well-being: some cause much less harm than others.
On this page, you can find a list of key insights as well as a list of visualizations on illicit drug use. This provides a global overview of illicit drug use, dependency disorders, and some of their impacts.
Key Charts on Illicit Drug Use
See all charts on this topicEndnotes
Babor, Caulkins, and Edwards (2010) – Drug policy and the public good. Oxford University Press.
United Nations International Drug Control Programme. Laboratory Section. (2016). Terminology and information on drugs: third edition. United Nations Publications.
Maclean, J. C., Mallatt, J., Ruhm, C. J., & Simon, K. (2021). Economic studies on the opioid crisis: A review. National Bureau of Economic Research.
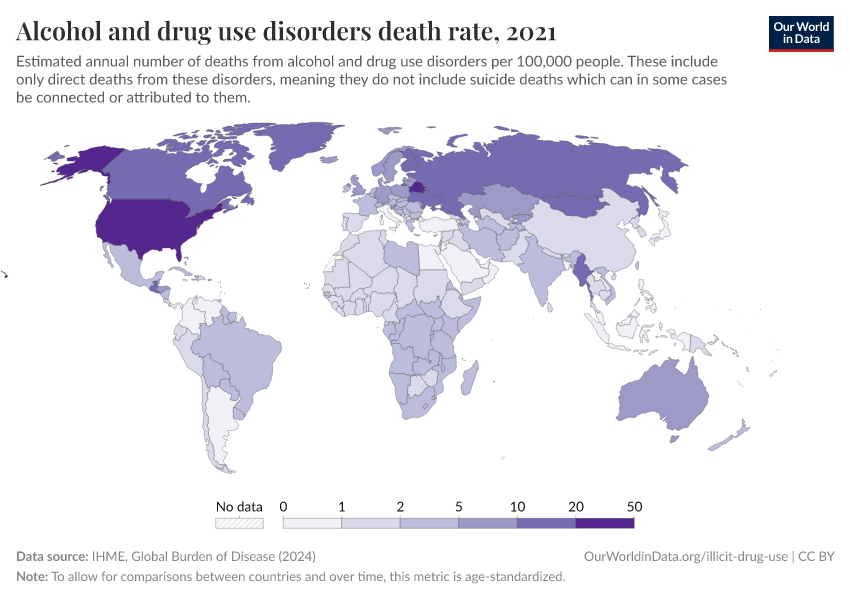
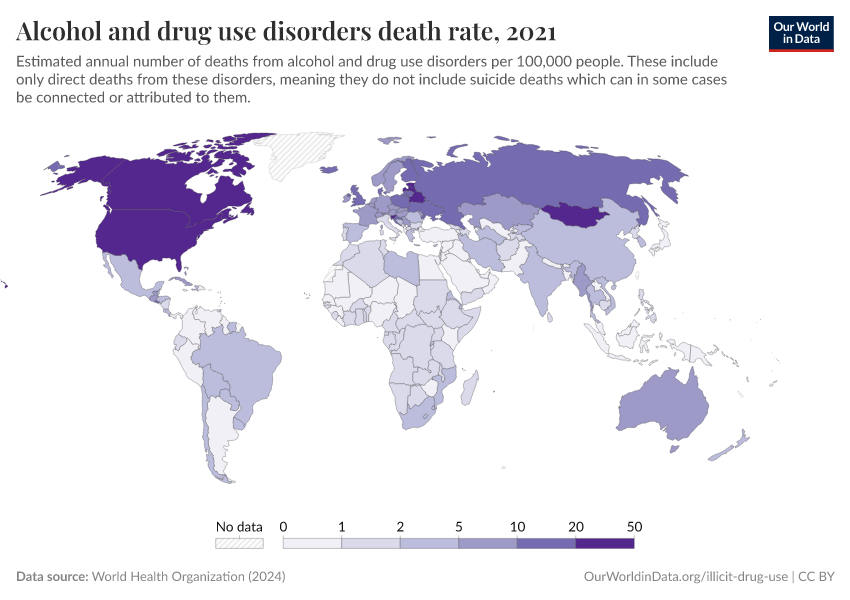
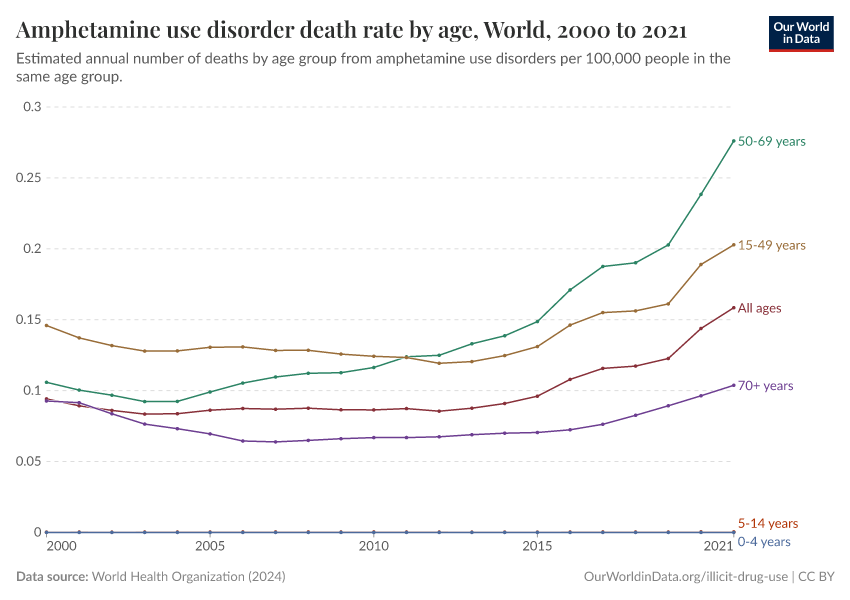
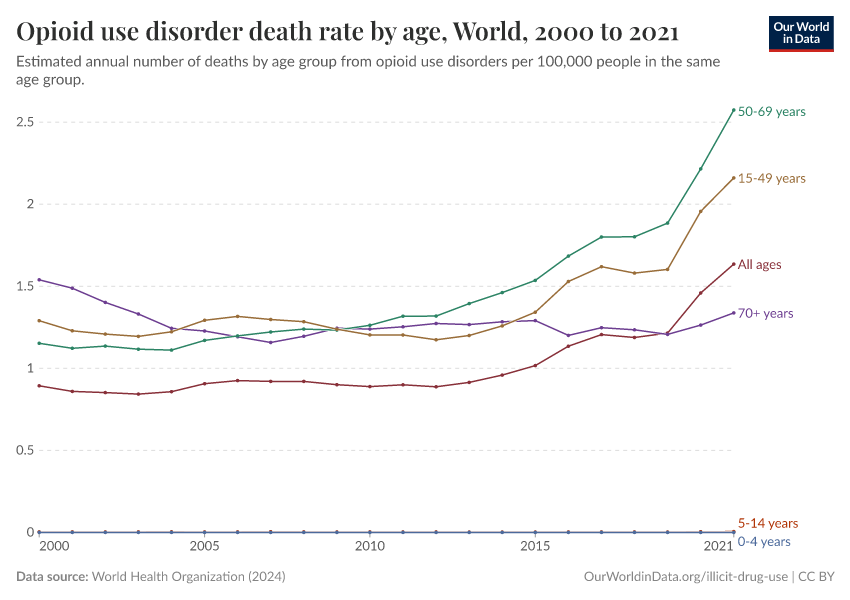
Note that these figures are age-standardized (which means they assume a constant age structure of the population over time) whereas the previous key insight showed figures that were not age-standardized.
Cite this work
Our articles and data visualizations rely on work from many different people and organizations. When citing this topic page, please also cite the underlying data sources. This topic page can be cited as:
Hannah Ritchie, Pablo Arriagada, and Max Roser (2022) - “Opioids, Cocaine, Cannabis, and Other Illicit Drugs” Published online at OurWorldinData.org. Retrieved from: 'https://ourworldindata.org/illicit-drug-use' [Online Resource]BibTeX citation
@article{owid-illicit-drug-use,
author = {Hannah Ritchie and Pablo Arriagada and Max Roser},
title = {Opioids, Cocaine, Cannabis, and Other Illicit Drugs},
journal = {Our World in Data},
year = {2022},
note = {https://ourworldindata.org/illicit-drug-use}
}Reuse this work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
All of our charts can be embedded in any site.