Pneumonia — no child should die from a disease we can prevent
How many children die from pneumonia? How has this changed over time, and how can we prevent it?
Every 39 seconds a child dies from pneumonia.1 By the time you finish reading this post at least five children will have died from it. For a disease we know how to treat and prevent, this should never be the case.
Pneumonia is the leading cause of child mortality
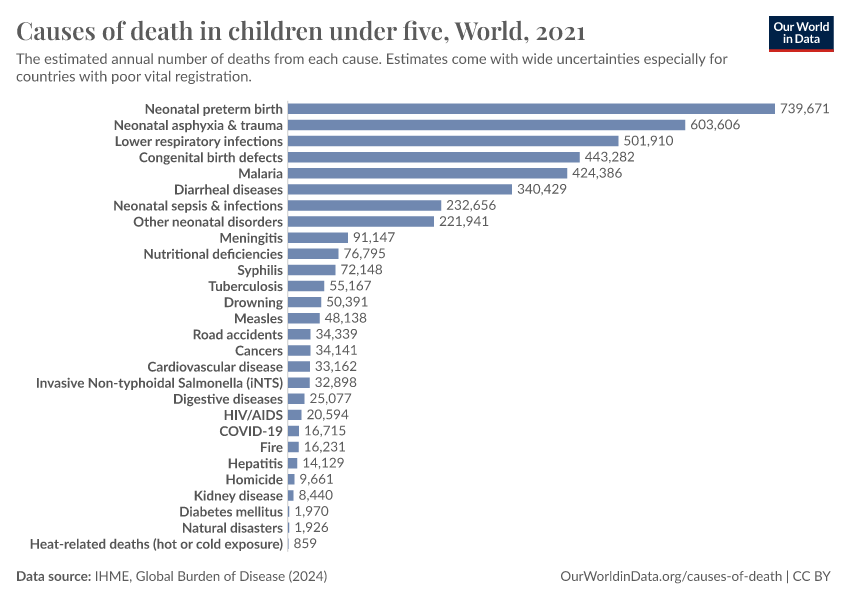
5.4 million children under five years old died in 2017. Pneumonia was the cause of death of one-in-seven of them.2 As the visualization shows, pneumonia is the leading cause of child mortality globally and has been the leading cause for the past three decades.
Today more than 2000 children will die from pneumonia
809,000 children under five years old died from pneumonia in 2017. This means, on average, the disease claimed more than 2,200 children every day.3
As the map shows, children are most likely to die from pneumonia across Sub-Saharan Africa and South Asia. Just 5 countries — India, Nigeria, Pakistan, the Democratic Republic of Congo, and Ethiopia – accounted for more than half of all deaths from childhood pneumonia in 2017.
In a 2018 comment in the journal Lancet, Kevin Watkins and Devi Sridhar called pneumonia “the ultimate disease of poverty”.4 There is a strong correlation between a country’s income and child mortality from pneumonia. Pneumonia is not a disease that transmits easily across borders; it is generally restricted to local communities and can be controlled when basic health measures are available. The disease is therefore most common in places where healthcare infrastructure is lacking and people are least able to afford treatment.5

We’ve made enormous progress against pneumonia, but many more lives could be saved
In the visualization here we see global deaths from pneumonia by age group. The number of children dying from pneumonia has decreased substantially over the past three decades. In 1990, more than two million children died from pneumonia each year; by 2017 this number had fallen by almost two-thirds.
As well as increased availability of interventions and treatments such as pneumococcal vaccines and antibiotics, improvements in the major risk factors such as childhood wasting, high air pollution, and poor sanitation have all contributed to this decline. By continuing to reduce child exposure to these risk factors we can continue to reduce child mortality from pneumonia. We explore the role of these risk factors in more detail here.
Apart from limiting risk factors, one of the best ways to prevent pneumonia is to vaccinate children against the pathogens that cause it – and we have very effective vaccines available. PCV and Hib vaccines protect children from pneumonia caused by pneumococcus and H. influenzae. Researchers have estimated that, combined, these vaccines saved the lives of 1.4 million children between the years of 2000 and 2015.6
But still too few children are vaccinated, which means we are missing out on the much greater impacts vaccines could have. Cynthia Chen et al. (2019) suggest that if almost every child would be immunised with pneumococcal vaccine, we could save the lives of close to 400,000 children annually.7 We discuss the potential of pneumococcal vaccines in more detail here.
In addition to vaccination, promoting breastfeeding of newborns is also an essential preventative measure. Research by Laura Lamberti et al. (2013) suggests mortality from pneumonia in lower-income countries among children who are not breastfed in the first 5 months of their lives is 15 times greater than those who exclusively received their mother’s milk.8
And when prevention is not sufficient, we need to provide more access to available treatments. Better access to healthcare facilities, antibiotics, and oxygen therapy can all contribute to saving more lives.

In 1902 William Osler, one of the founders of Johns Hopkins Hospital and a pioneer medical teacher, referred to pneumonia as “Captain of the Men of Death”. In the early 20th century there were few treatments for pneumonia available; in the 1940s medical textbooks would still recommend bloodletting as one of them.9 Today we know the causes of the disease, what risk factors make children more likely to get the disease and we have multiple ways we can prevent and treat it. Many of the interventions we have today not only protect children from pneumonia but also help to limit diseases such as diarrhea, meningitis, tuberculosis, and others.
Pneumonia today is no longer a Captain — we know how to steer the course of the disease. But with all the tools we have at our disposal, there is still much work left to be done to save the 800,000 children lost each year due to this preventable disease.
Endnotes
Global Burden of Disease studies estimates that 809,000 children died from pneumonia in 2017. A typical year has 3.154*107 seconds. 3.154*107 / 809,000 = 39 seconds
The research literature uses the terms pneumonia and lower respiratory infections (LRIs) interchangeably. The Institute for Health Metrics and Evaluation (IHME) provides mortality data on LRIs, which they define as pneumonia caused by a range of different pathogens (see IHME (2014) and McAllister (2019) references), though they also include bronchiolitis in this category. In this entry we use data provided by IHME as an estimate for the deaths from pneumonia. While cases of bronchiolitis are quite common they are generally not fatal, therefore, it is reasonable to assume that most of IHME data refers to cases of clinical pneumonia.
Clinical pneumonia (also called WHO-pneumonia) is pneumonia that is diagnosed by symptoms (fast breathing and coughing). Symptoms-based definition inevitably means that diseases with similar symptoms may be misdiagnosed as clinical pneumonia.
Ideally, pneumonia would always be diagnosed by a physician using radiological imaging and by determining the causative agent. However, because such diagnosis requires a lot of resources, it is often not possible to do. Puumalainen et al. study from 2008 has found that 34% of clinically diagnosed pneumonia cases have radiographic evidence of pneumonia and 11% had a diagnosable bacterial cause.
Institute for Health Metrics and Evaluation (IMHE). (2014). Pushing the Pace: Progress and Challenges in Fighting Childhood Pneumonia.
McAllister, D. A., Liu, L., Shi, T., Chu, Y., Reed, C., Burrows, J., ... & Nair, H. (2019). Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis.The Lancet Global Health, 7(1), e47-e57.
Puumalainen, T., Quiambao, B., Abucejo-Ladesma, E., Lupisan, S., Heiskanen-Kosma, T., Ruutu, P., ... & Riley, I. (2008). Clinical case review: a method to improve identification of true clinical and radiographic pneumonia in children meeting the World Health Organization definition for pneumonia. BMC infectious diseases, 8(1), 95.
365 days in a year. In 2017 808,920 children died from pneumonia. On average, 808,920 / 365= 2,216 lives lost every day.
Watkins, K., & Sridhar, D. (2018). Pneumonia: a global cause without champions.The Lancet, 392(10149), 718-719.
The Lancet Global Health Editorial (2018). The disgraceful neglect of childhood pneumonia.The Lancet. Global health, 6(12), e1253.
Wahl, Brian, et al. "Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000–15."The Lancet Global Health 6.7 (2018): e744-e757.
Chen, C., Liceras, F. C., Flasche, S., Sidharta, S., Yoong, J., Sundaram, N., & Jit, M. (2019). Effect and cost-effectiveness of pneumococcal conjugate vaccination: a global modelling analysis.The Lancet Global Health, 7(1), e58-e67.
Lamberti, L. M., Zakarija-Grković, I., Walker, C. L. F., Theodoratou, E., Nair, H., Campbell, H., & Black, R. E. (2013). Breastfeeding for reducing the risk of pneumonia morbidity and mortality in children under two: a systematic literature review and meta-analysis.BMC public health, 13(3), S18.
Osler, William. The principles and practice of medicine. D. Appleton and Company, (1892-1942).
Cite this work
Our articles and data visualizations rely on work from many different people and organizations. When citing this article, please also cite the underlying data sources. This article can be cited as:
Bernadeta Dadonaite (2019) - “Pneumonia — no child should die from a disease we can prevent” Published online at OurWorldinData.org. Retrieved from: 'https://archive.ourworldindata.org/20260211-174736/child-deaths-from-pneumonia.html' [Online Resource] (archived on February 11, 2026).BibTeX citation
@article{owid-child-deaths-from-pneumonia,
author = {Bernadeta Dadonaite},
title = {Pneumonia — no child should die from a disease we can prevent},
journal = {Our World in Data},
year = {2019},
note = {https://archive.ourworldindata.org/20260211-174736/child-deaths-from-pneumonia.html}
}Reuse this work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
All of our charts can be embedded in any site.