Large amounts of antibiotics are used in livestock, but several countries have shown this doesn’t have to be the case
Overuse is a risk for antibiotic resistance, but there are ways to reduce it.
For humanity, antibiotics are a huge blessing. Antibiotics have saved millions of lives from bacterial infections. However, there is growing concern that these bacteria will become resistant to the drugs we use against them.
When we think about antimicrobial resistance, we often focus on what drugs humans take. We might not even consider the use of antibiotics in livestock, but they also pose a threat.
In fact, much more antibiotics are given to livestock than to humans. Researchers previously estimated that, in the 2010s, around 70% of antibiotics used globally were given to farm animals..1 While there hasn’t been an update of these figures in the last few years, it’s likely that more antibiotics are still used in livestock than humans.
Overusing antibiotics in livestock increases the risk of disease in animals and humans in several ways. First, antibiotics are often used as a cheap substitute for basic animal welfare practices, such as giving animals enough space, keeping their living environments clean, and ensuring that barns are well-ventilated.2 A failure to maintain hygienic conditions on farms increases the risk of disease for both livestock and humans.
The overuse of antibiotics can also increase the risk of bacteria that are resistant to treatment. That threatens the health of the animals but can also be a risk for humans for crossover diseases — diseases that also occur in humans, and we can treat with antibiotics. Finally, humans can be exposed to resistant pathogens by eating contaminated meat and dairy products.
To reduce the risks of antibiotic resistance, we don’t have to only consider the use of antibiotics in humans but also how to use them more effectively in the meat and dairy sector.
We know that this can be done: there are clear success stories of countries that have done so while maintaining healthy and productive meat and dairy industries.
In this article, we look at antibiotic use in livestock worldwide and what can be done to reduce it.
Pigs, chickens, and cattle use very different amounts of antibiotics
One of the key challenges in understanding the extent and risks of antibiotic resistance in livestock is the lack of transparent data sharing from countries. We go into more detail on this in a separate article.
While we don’t have high-quality data for many countries in the world, we can still understand the usage of different types of animals from countries that monitor and report their data transparently.
Intensive livestock consumes four times the amount of antibiotics compared to livestock raised outdoors. However, the amount of antibiotics used in different animals varies a lot.
Of course, comparing the total amount of antibiotics given to cows, sheep, pigs, and chickens would be unfair. Cows are bigger than chickens, so we’d expect them to need more antibiotics for the same impact (just as adults tend to need larger doses of medicine than children).
So, researchers compare antibiotic use in units adjusted for the size of animals — usually as the number of milligrams used per kilogram of meat product.
Chickens tend to receive the least antibiotics. You can see this in the chart below: they receive about seven times less than sheep and five times less than pigs.3 Cows also receive less than pigs and sheep.
Of course, the exact amount of antibiotics given varies across countries — as we’ll soon see. However, even within countries, the rankings of animal antibiotic use remain the same.
One of the reasons why antibiotics are used in lower quantities in chickens is that they are killed at a much younger age. Fast-growing breeds reach their “slaughter weight” at around 42 days, so they’re often slaughtered when they’re just 40 to 50 days old. Since their lifespan is shorter, they consume fewer antibiotics. Pigs are usually slaughtered at a slightly older age when they’re around five to six months.
The fact that intensive livestock get far more antibiotics than animals raised outdoors is one reason why cows tend to get less antibiotics than pigs. Although many cows are raised intensively in feedlots for some portion of their life, they tend to spend more of their lives outdoors than pigs, in less intensive conditions.
Antibiotic use differs hugely between countries
There are also massive gaps across countries.
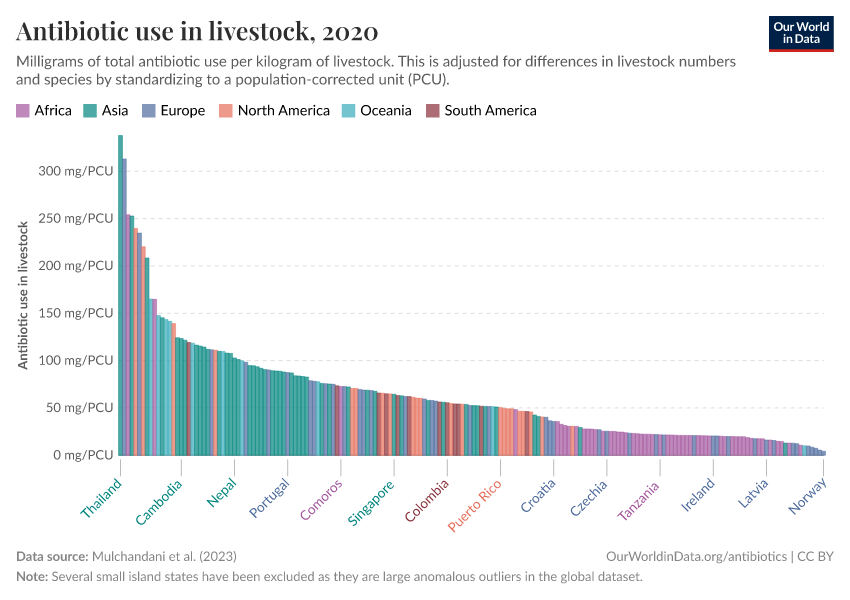
Researchers Ranya Mulchandani and colleagues estimated antibiotic use across the world based on the best available data, as well as extrapolations for those countries that don’t release data.3
The chart below shows their results; each bar represents a country. We have the most intense antibiotic users on the left, and on the right, we have the least intense. The figures are given in milligrams per kilogram of meat produced, which adjusts for the size of animals.
Thailand uses 80 times as much antibiotics for livestock as Norway.
Each bar is colored by region. You can see that most of the bars on the left — the most intense users — tend to be in Asia, with a few in the Americas or Oceania. But most clearly, on the right, we see European and African countries. They tend to use far less than other regions.
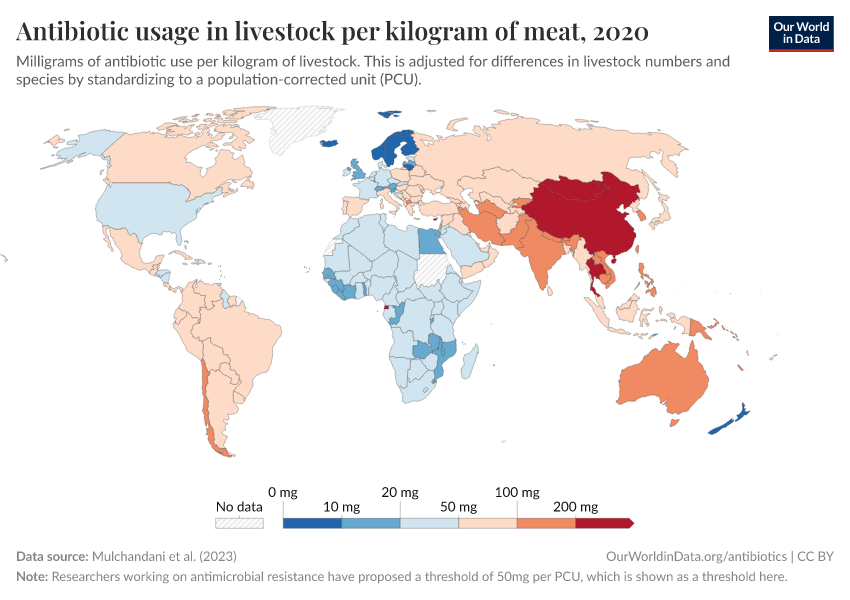
The map below shows the same data. Asia, Oceania, and most of the Americas use a lot of antibiotics. Europe and Africa, in blue, tend to use less than 50 milligrams per kilogram.
You can also see this when we look at regional averages.
In the bar chart, you can see this given as a regional average. Again, the intensity of antibiotic use is highest in Asia, followed by the Americas, Africa, and then Europe.
There are a few reasons why these differences are so large.
The first one is affordability and access: farmers in Africa, for example, have less access, just like they have less access to other farming inputs, such as fertilizers or pesticides.
Another reason is the differences in regulatory and industry norms regarding antibiotic use. As I’ll discuss later, antibiotic use has dropped significantly in Europe, partly due to regulation.
Finally, the most popular types of livestock make a difference. As we saw earlier, sheep and pigs tend to receive far more antibiotics than cattle or chickens, even after adjusting for their size.
That means countries that raise many pigs would tend to use more antibiotics. More than half of Thailand’s meat supply is in the form of pigmeat. In China, it’s two-thirds. That’s more than the global average of one-third and more than most other countries.
Some countries have reduced antibiotic use a lot
Antibiotics can play an important role in preventing disease and illness in animals. This is no different from humans. So, removing them completely is not necessarily the best option.
The key is to use them more effectively: changing farming practices to reduce antibiotic use where it’s in excess, or there are alternative ways to prevent disease, and using antibiotics in smaller quantities when it is needed. Many antibiotics given today are not used to prevent disease but to promote growth and produce meat more efficiently.4
We know countries can reduce antibiotic use while maintaining healthy livestock sectors because some countries have already achieved rapid reductions.
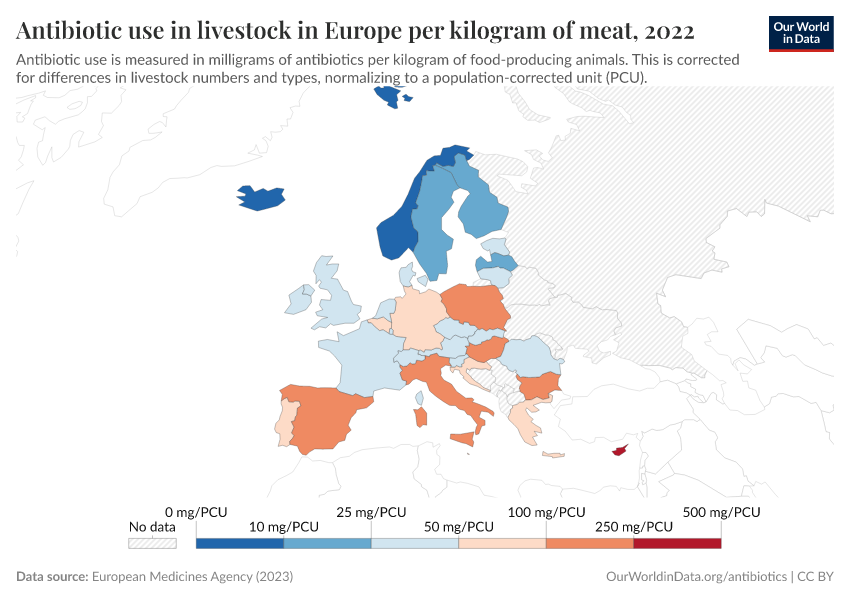
Several European countries have been particularly successful. You can see a big drop in antibiotic use in the chart below.
Between 2011 and 2022, sales of veterinary antibiotics — measured in tonnes — fell by more than half.5 The use of antibiotics considered critically important in human medicine also fell by half, with some specific drugs falling by 80% to 90%.

Regulation has played a crucial role.6 In many European countries, antibiotics today can only be administered with a prescription from a veterinarian.7 Vets are then given strict guidelines on how much and when they can be prescribed. Several countries — such as Denmark, Belgium, and France — have also imposed taxes or prohibited discounts on veterinary antibiotic sales, which reduces their incentives to prescribe them when they’re not essential.8
Other changes in the livestock sector have probably also played a role. Reducing the intensity of animal production might have reduced the need for antibiotics. Countries such as the Netherlands have started to move away from fast-growing to slower-growing chicken breeds; this improves animal welfare and reduces the need for antibiotics.9 Although animals tend to need fewer antibiotics when they have shorter lives (so that fast-growing breeds are “better” in this regard), the intensity of antibiotic use in slower-growing breeds is much lower and, therefore, results in a net reduction in the amount of antibiotics needed.
These countries have managed to decouple a healthy and productive livestock industry from antibiotic use
Farmers don’t spend money on antibiotics for no reason. They do it because they believe that it keeps their animals healthy and improves the profitability of their farm.
One of their key concerns is that reducing antibiotic use would affect their income and bottom line. But the evidence suggests otherwise. The dramatic reduction in antibiotic use in Europe gives us insight into how these reductions affect farm productivity.
A number of studies suggest that it did not affect economic performance. One study found that antibiotic use on pig farms in the Netherlands fell by 54% between 2004 and 2016, without negative impacts on animal welfare or economic results.10
Other interventions in Europe have found similar results: antibiotic use has fallen while animal health and farmer profit remained stable or, in some cases, increased.11
If we look at the amount of pigmeat produced per animal, we can see that it has been stable (or, in some cases, has continued increasing) in European countries. And most of these countries get higher yields than in China, which uses far more antibiotics. The same is true for chicken. And beef.
Decoupling antibiotic use from productivity doesn’t happen on its own. Farmers need to implement other strategies to manage disease and improve the living conditions of animals on the farm. These interventions include things like vaccinations, providing animals with more space and ventilation, and keeping equipment and feeding spots clean and disinfected.
Antibiotics have, in some sense, been a substitute for focusing on these alternative ways of managing animal health. But these exist and can be just as cost-effective.
More selective use of antibiotics, improved welfare practices, and eating less meat could reduce the risks of antimicrobial resistance
Reducing the intensity of antibiotic use in livestock is the clearest path to reducing overall antibiotic use and the health risks of antimicrobial resistance.
Thomas van Boeckel and colleagues previously studied the impact of setting global guidelines to have antibiotic use below 50 milligrams per PCU.2. That’s around half the global average today. In the map below, you can see which countries fall below or above this suggested global guideline.
Most countries are above it, but it’s not unachievable: 50 mg per PCU is far higher than the quantities used in many European countries, New Zealand, and the United States.
If the world achieved this, then antibiotic use in livestock would fall between half and two-thirds.
Implementing other strategies to control and reduce disease in livestock can help with this. Basic welfare practices such as making sure that feeding and watering troughs are emptied regularly; disinfecting farm equipment; changing bedding, straw, or other materials; providing adequate ventilation in indoor sheds or barns; and giving animals enough space can all reduce the risk of disease spread, and the need for antibiotics. It improves the lives of the animals, too.

The other way to reduce total antibiotic use is to reduce overall meat consumption. Fewer animals being farmed means less use of antibiotics. As I’ve written elsewhere, this would help across several other environmental problems, including climate change, land use, deforestation, and biodiversity loss.
If meat consumption was reduced to 40 grams per person per day — equivalent to a thin beef patty — then antibiotic use could fall by two-thirds.12 Americans currently eat four to five times as much meat as this, so it would require pretty radical shifts in their diets.
Of course, doing both — cutting the intensity of antibiotic use and reducing meat consumption — would lead to even more dramatic declines in antibiotic use.
Acknowledgments
Many thanks to Max Roser and Edouard Mathieu for their comments on this article, and to Thomas van Boeckel for discussion and feedback.
Endnotes
Getting a definitive figure here is difficult because of data reporting and transparency issues, which I will describe later.
Several of the largest studies on antimicrobial use in livestock cite a figure of 72% or 73%. This appears to come from a study by Thomas van Boeckel and colleagues, published in 2017.
It estimates that the intensity of antimicrobial use in humans is around 118 mg per kg. And 133 mg per kg in animals. When we multiply these figures by the estimated biomass (i.e., the weight) of humans and livestock, we get a total estimate for humans of around 35,000 tonnes a year, compared to 85,000 tonnes in livestock. That would mean livestock accounted for around 72% of total antibiotic use.
A more recent study by Katie Tiseo and colleagues (2020) estimated that 66% of antimicrobials were used in livestock.
Van Boeckel, T. P., Pires, J., Silvester, R., Zhao, C., Song, J., Criscuolo, N. G., ... & Laxminarayan, R. (2019). Global trends in antimicrobial resistance in animals in low-and middle-income countries. Science.
Van Boeckel, T. P., Brower, C., Gilbert, M., Grenfell, B. T., Levin, S. A., Robinson, T. P., ... & Laxminarayan, R. (2017). Global trends in antimicrobial use in food animals. Proceedings of the National Academy of Sciences.
Mulchandani, R., Wang, Y., Gilbert, M., & Van Boeckel, T. P. (2023). Global trends in antimicrobial use in food-producing animals: 2020 to 2030. PLOS Global Public Health.
Tiseo, K., Huber, L., Gilbert, M., Robinson, T. P., & Van Boeckel, T. P. (2020). Global trends in antimicrobial use in food animals from 2017 to 2030. Antibiotics.
Van Boeckel, T. P., Brower, C., Gilbert, M., Grenfell, B. T., Levin, S. A., Robinson, T. P., ... & Laxminarayan, R. (2015). Global trends in antimicrobial use in food animals. Proceedings of the National Academy of Sciences.
Mulchandani, R., Wang, Y., Gilbert, M., & Van Boeckel, T. P. (2023). Global trends in antimicrobial use in food-producing animals: 2020 to 2030. PLOS Global Public Health.
Scientists discovered that giving antibiotics to animals promoted growth as far back as the 1940s, but there’s still no consensus on why. There are a couple of key hypotheses: antibiotics might increase the absorption of nutrients by thinning the intestinal lining; nutrients are protected from being partially destroyed by bacteria; antibiotics prevent the formation of toxins by bacteria, which diverts less energy away from the animal itself; reductions in inflammation; and the prevention of subclinical infections, which would otherwise cost the animal energy to fight off.
Butaye, P., Devriese, L. A., & Haesebrouck, F. (2003). Antimicrobial growth promoters used in animal feed: effects of less well-known antibiotics on gram-positive bacteria. Clinical microbiology reviews.
Miyakawa, M. E. F., Casanova, N. A., & Kogut, M. H. (2024). How did antibiotic growth promoters increase growth and feed efficiency in poultry?. Poultry Science.
European Medicines Agency, European Surveillance of Veterinary Antimicrobial Consumption, 2022. 'Sales of veterinary antimicrobial agents in 31 European countries in 2022' (EMA/299538/2023).
Speksnijder, D. C., Mevius, D. J., Bruschke, C. J. M., & Wagenaar, J. A. (2015). Reduction of veterinary antimicrobial use in the Netherlands. The Dutch success model. Zoonoses and public health.
Waluszewski, A., Cinti, A., & Perna, A. (2021). Antibiotics in pig meat production: Restrictions as the odd case and overuse as normality? Experiences from Sweden and Italy. Humanities and Social Sciences Communications.
This can be requested for individual animals or a group of animals in certain cases. Schmerold, I., van Geijlswijk, I., & Gehring, R. (2023). European regulations on the use of antibiotics in veterinary medicine. European journal of pharmaceutical sciences.
Sternberg-Lewerin, S., Boqvist, S., Nørstebø, S. F., Grönthal, T., Heikinheimo, A., Johansson, V., ... & Wasteson, Y. (2022). Nordic Vets against AMR—An Initiative to Share and Promote Good Practices in the Nordic–Baltic Region. Antibiotics.
Fortané, N. (2019). Veterinarian ‘responsibility’: conflicts of definition and appropriation surrounding the public problem of antimicrobial resistance in France. Nature Humanities and Social Sciences Communications.
Statens Serum Institute (2019). DANMAP 2018 - Use of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from food animals, food and humans in Denmark.
Wageningen University and Research. Economics of antibiotic usage on Dutch farms (2019). The impact of antibiotic reduction on economic results of pig and broiler farms in the Netherlands.
van Asseldonk, M., de Lauwere, C., Bonestroo, J., Bondt, N., & Bergevoet, R. (2020). Antibiotics use versus profitability on sow farms in the Netherlands. Preventive veterinary medicine.
Collineau, L., Rojo-Gimeno, C., Léger, A., Backhans, A., Loesken, S., Nielsen, E. O., ... & Krebs, S. (2017). Herd-specific interventions to reduce antimicrobial usage in pig production without jeopardising technical and economic performance. Preventive veterinary medicine. Postma, M., Vanderhaeghen, W., Sarrazin, S., Maes, D., & Dewulf, J. (2017). Reducing antimicrobial usage in pig production without jeopardizing production parameters. Zoonoses and public health. Rojo-Gimeno, C., Postma, M., Dewulf, J., Hogeveen, H., Lauwers, L., & Wauters, E. (2016). Farm-economic analysis of reducing antimicrobial use whilst adopting improved management strategies on farrow-to-finish pig farms. Preventive Veterinary Medicine.
A Big Mac patty in McDonald’s is around 40 grams. Most burger patties are much thicker than this: often double or triple the weight.
Cite this work
Our articles and data visualizations rely on work from many different people and organizations. When citing this article, please also cite the underlying data sources. This article can be cited as:
Hannah Ritchie and Fiona Spooner (2024) - “Large amounts of antibiotics are used in livestock, but several countries have shown this doesn’t have to be the case” Published online at OurWorldinData.org. Retrieved from: 'https://archive.ourworldindata.org/20251209-133038/antibiotics-livestock.html' [Online Resource] (archived on December 9, 2025).BibTeX citation
@article{owid-antibiotics-livestock,
author = {Hannah Ritchie and Fiona Spooner},
title = {Large amounts of antibiotics are used in livestock, but several countries have shown this doesn’t have to be the case},
journal = {Our World in Data},
year = {2024},
note = {https://archive.ourworldindata.org/20251209-133038/antibiotics-livestock.html}
}Reuse this work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
All of our charts can be embedded in any site.