How do researchers study the prevalence of mental illnesses?
Global data on mental health is essential to understand the scale and patterns of these illnesses, and how to reduce them. How do researchers collect this data, and how reliable is it?
In many countries, many people with mental illnesses go undiagnosed, meaning mental health is given less attention and support than it deserves. Even for those diagnosed, treatment can be of poor quality, if they receive it at all.1
To reduce the burden of mental illnesses, the world needs reliable data, which includes the number of people that face mental illnesses, how and when they occur, and the effectiveness of treatments.
How are mental illnesses defined?
Defining mental illnesses is complex. They are diagnosed based on people’s psychological symptoms and behavior rather than biomarkers, brain scans, or blood tests. This makes them more subjective – they are dependent on whether people share their symptoms and the way doctors diagnose them.
Mental illnesses are formally defined according to the International Classification of Diseases (ICD) and the Diagnostic and Statistical Manual of Mental Disorders (DSM). The ICD is used internationally by healthcare professionals, while the DSM is primarily used by psychiatrists in the United States.2
These manuals explain how to diagnose mental illnesses by observing and asking about people’s symptoms and behavior, and the context of their symptoms – for example, symptoms that appeared because of drug use or other medical conditions don’t qualify as mental illnesses.
Based on these definitions, healthcare professionals can make diagnoses, which can be used for healthcare, treatment, and national statistics.
Over time, the definitions of particular mental illnesses have changed. The DSM has been revised 5 times since it was first developed in 1952, while the ICD has been revised 11 times since 1900.3 They will continue to be revised in the future, but updates have become less frequent.
Their changes are partly due to a better understanding and measurement of mental illnesses. They have also changed as a result of cultural and legal factors. There used to be larger differences in the criteria for diagnosing mental illnesses between the ICD and the DSM, but the two manuals are now more similar due to collaboration between their developers.4
Mental health data based on diagnoses
The process of diagnosing a mental illness usually starts with the patient consulting a healthcare professional.5 This can be a doctor in a clinic or general hospital, a psychiatrist, or another mental health specialist.
Health professionals use official medical guidance and professional judgment to decide whether to diagnose a patient with a condition.
Data on these diagnoses are collected from hospitals in many countries, but this may not include clinic visits. The data can include people’s age and sex, their reason for admission, other diagnoses, and treatments given during their visit.6
What are the strengths and limitations of diagnosis data?
Strengths of data based on diagnosis
Official data from diagnoses of mental illnesses have two major strengths.
First, the diagnoses come from healthcare professionals with training and experience in recognizing mental illnesses.
They can use their knowledge to ask people more questions about their symptoms and understand their context before making a diagnosis. They can also perform additional medical tests to rule out other conditions.
Second, data on diagnoses can tell us about the number of people who seek out mental health treatment from public hospitals and clinics. This can usually be linked to data on which treatments they were prescribed and for how long.7
This can be very useful for countries to understand the resources used to treat mental illnesses.
Limitations of data based on diagnosis
Data on diagnoses of mental illnesses also has limitations.
One problem is that many people do not reach out to healthcare professionals about their health conditions. This might be because they lack awareness of mental illnesses or there is a lack of healthcare for these conditions in their country. They may also feel uncomfortable about sharing their symptoms with healthcare professionals.
Another problem is that the diagnoses may not be made consistently. Doctors can have different levels of training and experience in recognizing and diagnosing mental illnesses. This can be a problem when comparing diagnosis rates between countries.
A third problem is that national data on diagnosis is often collected from a limited number of sources. Data from private hospitals and clinics is usually not included. In some countries, mental health data is collected from hospitals but not clinics.8
Some countries also use data from other sources. For example, the data might come from health insurance claims—which include private healthcare—or from other databases connected to many healthcare clinics across the country.
The final problem is that countries may use different definitions to diagnose patients. Some countries use modified versions of the ICD manual to collect their data, depending on their cultural context and needs.9
These differences mean that comparing data between countries using data on diagnoses can be difficult.
Mental health data based on surveys
Aside from the formal diagnoses, mental illnesses can be measured using surveys and screening questionnaires.
These tend to ask people about symptoms similar to those in diagnostic manuals, but they can be used more easily and widely because the data does not need to be collected by a healthcare professional.
These surveys can be conducted in different ways: over the phone, online, or in-person while anonymized.10
During the surveys, trained professionals ask people in the general population whether they have experienced symptoms of mental illnesses. They also ask about the age when people first experienced them, how long they lasted, and how severe the symptoms were.
People may be asked about symptoms they have currently, or have had recently, or in their lifetime so far.
Some symptoms of mental illnesses may be common in the population. This chart shows data from a US survey called the National Health and Nutrition Examination Survey. It was a large-scale, in-person survey of people in the general population.11
As you can see, around a fifth of the US population says they have had a depressed mood for several days in the past two weeks.
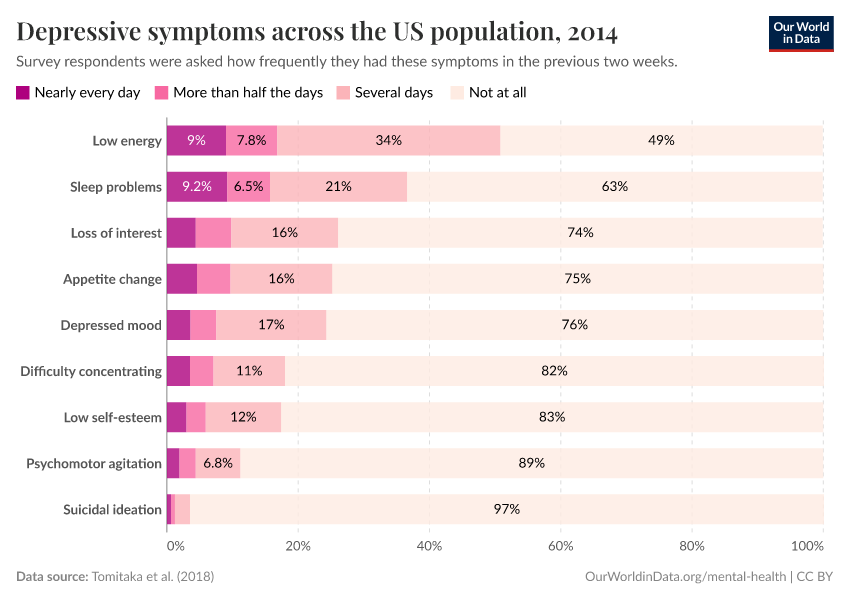
But having one or a few symptoms does not necessarily mean that someone can be diagnosed with depression. Instead, researchers look at the combination of symptoms that people report. They will set a threshold for the number of symptoms someone must have before they are considered to have the condition.
To diagnose someone with major depression, for example, the ICD and DSM criteria require them to have had a depressed mood or loss of interest for much of the day, nearly every day, for at least two weeks, along with several other symptoms.
What are the strengths and limitations of survey data?
Strengths of survey data
Survey data on mental health has two major strengths.
First, it involves structured interviews – people are asked a consistent set of questions regardless of their interviewer. This helps to ensure the data is more comparable between interviewers and across time.12
Second, surveys include a much wider range of people in the population, including those who would not seek treatment due to a lack of awareness, costs, or other concerns.
This can help to understand the prevalence of mental illnesses in the general population, including people never diagnosed by a healthcare professional. This can help us understand what share of people seek treatment.
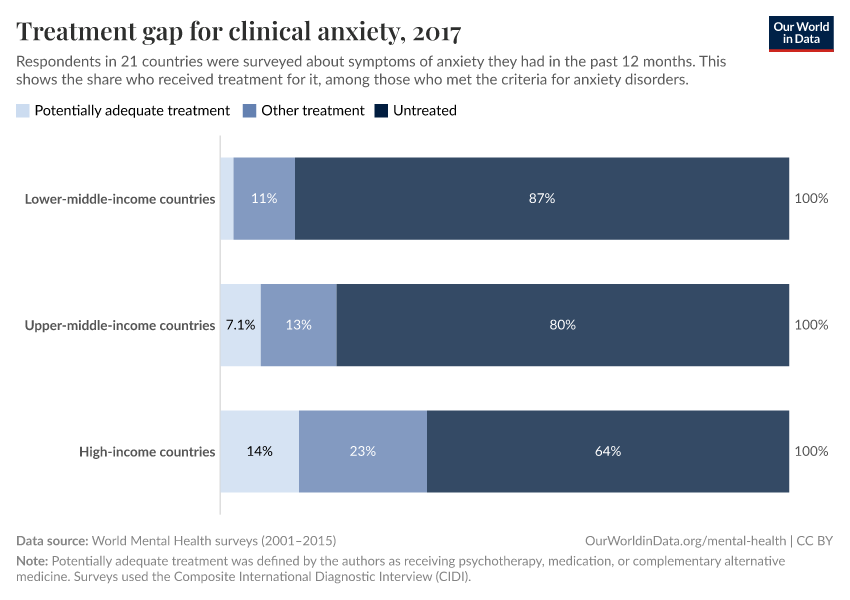
One example is the World Mental Health surveys: these were large-scale surveys of mental illnesses in the general population in 21 countries of different income levels.13
Based on structured interviews, the authors found that around 1 in 10 people met the criteria for an anxiety disorder in the past year across countries surveyed.14
In the chart, you can see the share of those who met the criteria who also said they had received treatment. Only around 36% with anxiety disorders received any treatment in high-income countries, while an even lower share – only 13% – received it in lower-middle-income countries.15
Third, surveys can tell us about milder symptoms that may be common in the population. This can help to see if a condition lies on a spectrum – where everyone has the symptoms to different degrees – or if it affects a separate share of people.
Limitations of survey data
There are also several limitations of survey data to keep in mind.
One is that people may not share their symptoms in surveys, as they may not feel comfortable sharing them with researchers. Along with this, people’s comfort in sharing mental health symptoms may vary between countries and over time.16
Another limitation is that people may not remember their symptoms, especially when they are asked to recall symptoms in their lifetime so far. This can be challenging for older people whose symptoms may have occurred decades ago.
This chart shows data from a study where the same people were interviewed several times about depression in their lifetimes so far.17 Around two-thirds of people who had described episodes of depression did not recall them in subsequent interviews.
A third limitation is that survey data does not usually exclude other diagnoses. When people visit a doctor for a diagnosis, the doctor may ask them about other existing conditions and medications they are taking, and test them for other medical conditions which could also cause their symptoms. This is not usually performed in surveys.
It can also be difficult to compare people’s responses in surveys, because people may interpret the questions differently. This can make it difficult to compare people from different backgrounds, languages, and countries.18
Another consideration is who is included in surveys. Some include people from a wide range of backgrounds in the general population, while others only include particular groups like urban residents or university students.
This can be a big problem for mental health conditions that are less common, such as schizophrenia and bipolar disorder. If only a few people in the study had a condition, then it can be difficult to estimate the precise share of the total population with it.
It’s also important to know that surveys of the general population usually do not include people who are institutionalized in hospitals or prisons, who may have more severe physical and mental health conditions.19
How much data on mental health is available around the world?
Data on mental health varies in two ways: the amount of data on each mental illness and the amount of data from each country.
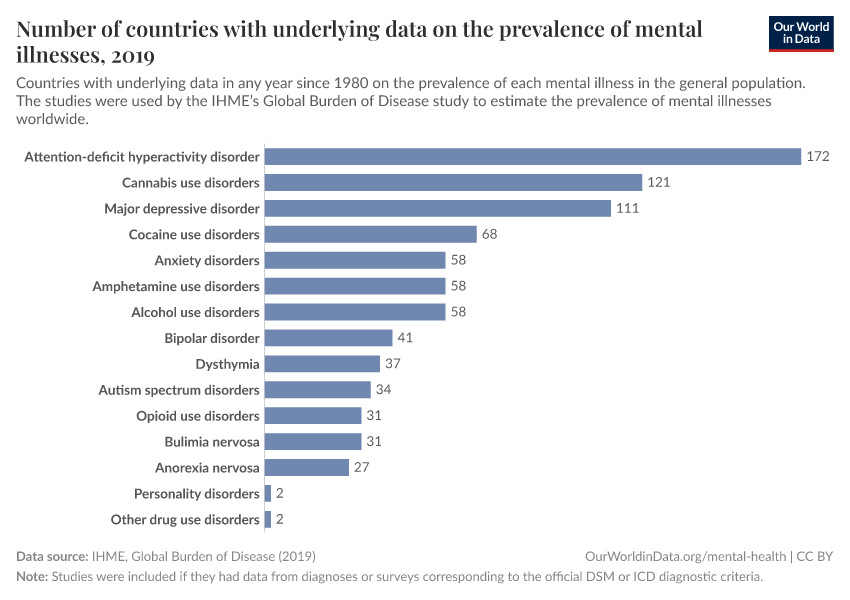
First, there is much more data available on some mental illnesses than others.
You can see this in the chart. It shows the number of countries with primary data on the prevalence of each mental illness in the general population. The studies were used by the IHME’s Global Burden of Disease study to estimate the prevalence of mental illnesses worldwide.20
As you can see, data on some mental illnesses such as attention-deficit hyperactivity disorder, cannabis use disorder, and major depressive disorder came from a large number of countries.
However, data on others, such as bipolar disorder, autism spectrum disorders, and anorexia nervosa, came from fewer than 40 countries. For personality disorders, data came from only two countries.
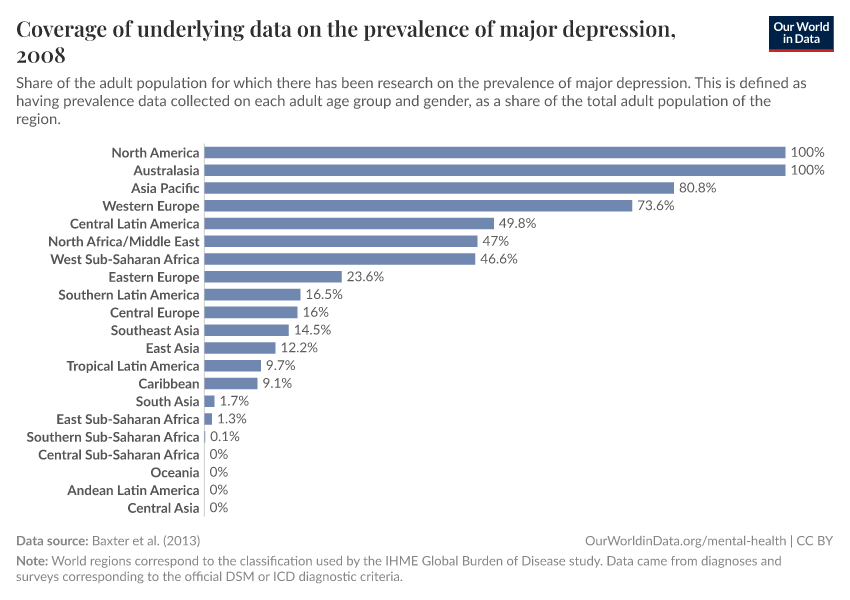
Second, there is much more data available from some world regions than others.
In the left-hand chart, you can see the share of the population of world regions that had any data collected on the prevalence of major depression between 1980 and 2008.
This comes from an older study published in 2013, and more data has been collected since then, which has helped improve estimates made by the Global Burden of Disease study.8
In Australasia and North America, there was data relating to all of the age demographics in the population. But in regions such as Eastern Europe and Southeast Asia, less than 25% of the population was covered.
In several regions, especially in sub-Saharan Africa, Central Asia, and South America, there was almost no underlying data available.
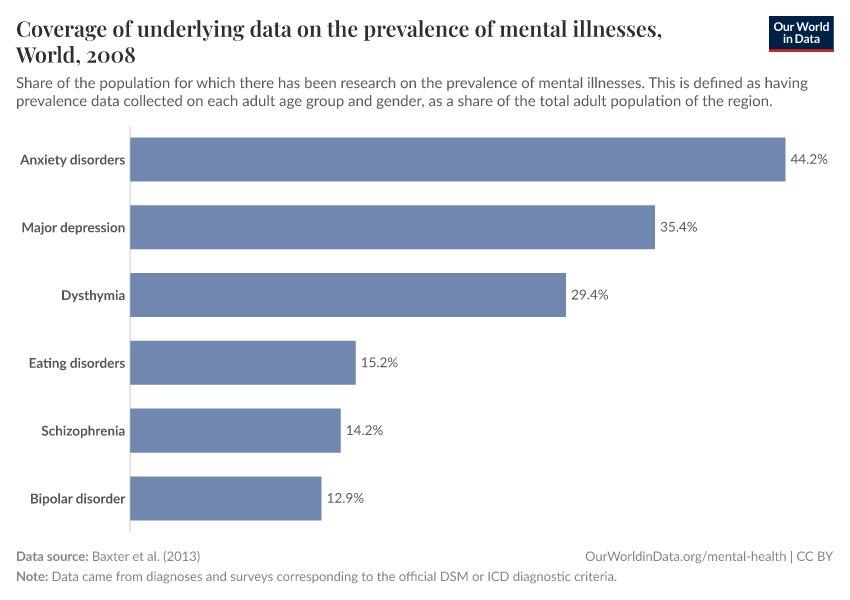
What about other mental illnesses apart from depression?
In the chart, you can see the population that was covered in data on other common mental illnesses.
As you can see, there was more data available on anxiety disorders and major depression than on schizophrenia and bipolar disorder.
You can click ‘Change country’ to see how this varies between world regions.
How do researchers extrapolate this data to make comparable estimates?
Researchers can try to make comparable estimates of mental health using this underlying data and statistical methods.21
These methods incorporate the available data on people’s mental health, their demographics, and the level of diagnosis and testing. Then they extrapolate the results to other countries, where data has not been collected. This can be based on demographics such as age and sex, other risk factors, responses to other large-scale representative mental health surveys.22
They try to adjust for the fact that the underlying data was collected from different sources (diagnoses or surveys), during different periods, and from different groups of people.
However, they come with a range of uncertainty. This is because they rely on assumptions about how the data was collected, and why some demographics and countries lacked data on the prevalence of mental illnesses.
This is especially true for some illnesses – such as eating disorders and bipolar disorder – and some world regions – including much of Asia, South America and Africa; where primary data is lacking.
Data on global mental health is limited – but nevertheless gives us important insights
Data on global mental health has two main limitations.
First, our understanding of global mental health depends on people’s willingness to share their symptoms, and contact healthcare professionals to receive a diagnosis and treatment. Because of this, many people remain undiagnosed and lack support and treatment.
Another major limitation is that data is lacking in many countries. It is often available only for some age groups, and is collected by separate one-off studies at infrequent intervals. There is much less data available for some illnesses than others.
For countries that lack data, the prevalence of mental illnesses is estimated from other similar countries with data, but this leads to large uncertainties.
Despite these limitations, the available data does give us important insights:
Importantly it shows that mental illnesses are not uncommon. For example, the World Mental Health surveys estimated that one-in-ten people met the criteria for anxiety disorders in the past year, on average, across countries.14
Global data also tells us that mental illnesses have a large treatment gap, especially in poorer countries. For example, while around one-in-three with anxiety disorders received any treatment in high-income countries, less than one-in-eight did in lower-middle-income countries.
Mental illnesses are a major part of the global health burden and remain untreated for many people. To address this, countries need more data on these conditions for a wide range of demographics, and long-term data to understand how they develop, and how effective the treatments are.
Acknowledgements
I would like to thank Edouard Mathieu, Hannah Ritchie and Max Roser for their helpful suggestions to improve this article.
Endnotes
Alonso, J., Liu, Z., Evans‐Lacko, S., Sadikova, E., Sampson, N., Chatterji, S., ... & WHO World Mental Health Survey Collaborators. (2018). Treatment gap for anxiety disorders is global: Results of the World Mental Health Surveys in 21 countries. Depression and anxiety, 35(3), 195-208. https://doi.org/10.1002/da.22711
Kupfer, D. J., Regier, D. A., & Kuhl, E. A. (2008). On the road to DSM-V and ICD-11. European Archives of Psychiatry and Clinical Neuroscience, 258(S5), 2–6. https://doi.org/10.1007/s00406-008-5002-6
American Psychiatric Association. (2022). DSM History. https://www.psychiatry.org/psychiatrists/practice/dsm/about-dsm/history-of-the-dsm
Hirsch, J. A., Nicola, G., McGinty, G., Liu, R. W., Barr, R. M., Chittle, M. D., & Manchikanti, L. (2016). ICD-10: History and Context. AJNR. American Journal of Neuroradiology, 37(4), 596–599. https://doi.org/10.3174/ajnr.A4696
This paper provides a detailed summary of the similarities and differences between the criteria for mental illnesses in the ICD-11 and DSM-5.
First, M. B., Gaebel, W., Maj, M., Stein, D. J., Kogan, C. S., Saunders, J. B., Poznyak, V. B., Gureje, O., Lewis‐Fernández, R., Maercker, A., Brewin, C. R., Cloitre, M., Claudino, A., Pike, K. M., Baird, G., Skuse, D., Krueger, R. B., Briken, P., Burke, J. D., … Reed, G. M. (2021). An organization‐ and category‐level comparison of diagnostic requirements for mental disorders in ICD ‐11 and DSM ‐5. World Psychiatry, 20(1), 34–51. https://doi.org/10.1002/wps.20825
Harrison, J. E., Weber, S., Jakob, R., & Chute, C. G. (2021). ICD-11: An international classification of diseases for the twenty-first century. BMC Medical Informatics and Decision Making, 21(S6), 206. https://doi.org/10.1186/s12911-021-01534-6
Tyrer, P. (2014). A comparison of DSM and ICD classifications of mental disorder. Advances in Psychiatric Treatment, 20(4), 280–285. https://doi.org/10.1192/apt.bp.113.011296
People can also be diagnosed through other routes. For example, in some countries, there are also screening programs to identify people who may have mental health conditions and refer them to specialists. Children and adolescents can be referred to healthcare professionals by carers.
In some countries, people can also be diagnosed and committed to mental hospitals involuntarily if they are considered to pose a danger to others. This was more common in countries like the United States before the 1960s, but since then, these laws have been reformed in many countries.
See also: Testa, M., & West, S. G. (2010). Civil commitment in the United States. Psychiatry (Edgmont (Pa.: Township)), 7(10), 30–40.
Zhang, S., Mellsop, G., Brink, J., & Wang, X. (2015). Involuntary admission and treatment of patients with mental disorder. Neuroscience Bulletin, 31(1), 99–112. https://doi.org/10.1007/s12264-014-1493-5
Appelbaum, P. S. (1997). Almost a revolution: an international perspective on the law of involuntary commitment. Journal of the American Academy of Psychiatry and the Law Online, 25(2), 135-147.
Otero Varela, L., Doktorchik, C., Wiebe, N., Quan, H., & Eastwood, C. (2021). Exploring the differences in ICD and hospital morbidity data collection features across countries: An international survey. BMC Health Services Research, 21(1), 308. https://doi.org/10.1186/s12913-021-06302-w
Varela, L. O., Knudsen, S., Carpendale, S., Eastwood, C., & Quan, H. (2019, October). Comparing ICD-Data Across Countries: A Case for Visualization?. In 2019 IEEE Workshop on Visual Analytics in Healthcare (VAHC) (pp. 60-61). IEEE.
In some countries, there are also national screening programs to diagnose patients with both physical and mental illnesses.
Baxter, A. J., Patton, G., Scott, K. M., Degenhardt, L., & Whiteford, H. A. (2013). Global Epidemiology of Mental Disorders: What Are We Missing? PLoS ONE, 8(6), e65514. https://doi.org/10.1371/journal.pone.0065514
Brhlikova, P., Pollock, A. M., & Manners, R. (2011). Global Burden of Disease estimates of depression – how reliable is the epidemiological evidence? Journal of the Royal Society of Medicine, 104(1), 25–34. https://doi.org/10.1258/jrsm.2010.100080
In-person surveys are usually anonymized for sensitive questions such as those on mental health. In this case, the person may be given a laptop to answer the questions while the interviewer cannot see their answers.
Tomitaka, S., Kawasaki, Y., Ide, K., Akutagawa, M., Yamada, H., Ono, Y., & Furukawa, T. A. (2018). Distributional patterns of item responses and total scores on the PHQ-9 in the general population: Data from the National Health and Nutrition Examination Survey. BMC Psychiatry, 18(1), 108. https://doi.org/10.1186/s12888-018-1696-9
Mueller, A. E., & Segal, D. L. (2014). Structured versus semistructured versus unstructured interviews. The encyclopedia of clinical psychology, 1-7. https://doi.org/10.1002/9781118625392.wbecp069
Kessler, R. C., Green, J. G., Gruber, M. J., Sampson, N. A., Bromet, E., Cuitan, M., ... & Zaslavsky, A. M. (2010). Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. International journal of methods in psychiatric research, 19(S1), 4-22. https://doi.org/10.1002/mpr.310
Alonso, J., Liu, Z., Evans-Lacko, S., Sadikova, E., Sampson, N., Chatterji, S., Abdulmalik, J., Aguilar-Gaxiola, S., Al-Hamzawi, A., Andrade, L. H., Bruffaerts, R., Cardoso, G., Cia, A., Florescu, S., de Girolamo, G., Gureje, O., Haro, J. M., He, Y., de Jonge, P., … the WHO World Mental Health Survey Collaborators. (2018). Treatment gap for anxiety disorders is global: Results of the World Mental Health Surveys in 21 countries. Depression and Anxiety, 35(3), 195–208. https://doi.org/10.1002/da.22711
Potentially adequate treatment was defined by the authors as receiving psychotherapy, medication, or complementary alternative medicine.
Gaia, A. (2020). Social Desirability Bias and Sensitive Questions in Surveys. In SAGE Research Methods Foundations. SAGE Publications Ltd. https://doi.org/10.4135/9781526421036928979
Krosnick, J. A. (1999). Maximizing questionnaire quality. Measures of Political Attitudes, 2, 37–58.
Shoemaker, P. J. (2002). Item Nonresponse: Distinguishing between don’t Know and Refuse. International Journal of Public Opinion Research, 14(2), 193–201. https://doi.org/10.1093/ijpor/14.2.193
Takayanagi, Y., Spira, A. P., Roth, K. B., Gallo, J. J., Eaton, W. W., & Mojtabai, R. (2014). Accuracy of Reports of Lifetime Mental and Physical Disorders: Results From the Baltimore Epidemiological Catchment Area Study. JAMA Psychiatry, 71(3), 273. https://doi.org/10.1001/jamapsychiatry.2013.3579
Putnick, D. L., & Bornstein, M. H. (2016). Measurement invariance conventions and reporting: The state of the art and future directions for psychological research. Developmental Review, 41, 71–90. https://doi.org/10.1016/j.dr.2016.06.004
Binswanger, I. A., Krueger, P. M., & Steiner, J. F. (2009). Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. Journal of Epidemiology & Community Health, 63(11), 912–919. https://doi.org/10.1136/jech.2009.090662
Peen, J., Schoevers, R. A., Beekman, A. T., & Dekker, J. (2010). The current status of urban-rural differences in psychiatric disorders. Acta Psychiatrica Scandinavica, 121(2), 84–93. https://doi.org/10.1111/j.1600-0447.2009.01438.x
Rehm, J., Kilian, C., Rovira, P., Shield, K. D., & Manthey, J. (2021). The elusiveness of representativeness in general population surveys for alcohol. Drug and Alcohol Review, 40(2), 161–165. https://doi.org/10.1111/dar.13148
Vos, T., Lim, S. S., Abbafati, C., Abbas, K. M., Abbasi, M., Abbasifard, M., Abbasi-Kangevari, M., Abbastabar, H., Abd-Allah, F., Abdelalim, A., Abdollahi, M., Abdollahpour, I., Abolhassani, H., Aboyans, V., Abrams, E. M., Abreu, L. G., Abrigo, M. R. M., Abu-Raddad, L. J., Abushouk, A. I., … Murray, C. J. L. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1204–1222. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30925-9/fulltext
Mathers, C., Hogan, D., & Stevens, G. (2019). Global health estimates: modelling and predicting health outcomes. The Palgrave handbook of global health data methods for policy and practice, 403-424. https://link.springer.com/chapter/10.1057/978-1-137-54984-6_21
Whiteford, H. A., Degenhardt, L., Rehm, J., Baxter, A. J., Ferrari, A. J., Erskine, H. E., ... & Vos, T. (2013). Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet, 382(9904), 1575-1586. https://doi.org/10.1016/s0140-6736(13)61611-6
Enders, C. K. (2022). Applied missing data analysis. Guilford Publications.
Rehm, J., & Shield, K. D. (2019). Global burden of disease and the impact of mental and addictive disorders. Current psychiatry reports, 21, 1-7. https://doi.org/10.1007/s11920-019-0997-0
Vos, T., Lim, S. S., Abbafati, C., Abbas, K. M., Abbasi, M., Abbasifard, M., Abbasi-Kangevari, M., Abbastabar, H., Abd-Allah, F., Abdelalim, A., Abdollahi, M., Abdollahpour, I., Abolhassani, H., Aboyans, V., Abrams, E. M., Abreu, L. G., Abrigo, M. R. M., Abu-Raddad, L. J., Abushouk, A. I., … Murray, C. J. L. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
For major depressive disorder, for example, the IHME uses available data on the age structure of the population; risk factors such as war mortality, intimate partner violence, and childhood sexual violence; as well as responses to the Gallup’s survey on negative experiences around the world. You can learn more in the Appendix of the Global Burden of Disease Study, which is available here.
Vos, T., Lim, S. S., Abbafati, C., Abbas, K. M., Abbasi, M., Abbasifard, M., Abbasi-Kangevari, M., Abbastabar, H., Abd-Allah, F., Abdelalim, A., Abdollahi, M., Abdollahpour, I., Abolhassani, H., Aboyans, V., Abrams, E. M., Abreu, L. G., Abrigo, M. R. M., Abu-Raddad, L. J., Abushouk, A. I., … Murray, C. J. L. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1204–1222. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30925-9/fulltext#supplementaryMaterial
Cite this work
Our articles and data visualizations rely on work from many different people and organizations. When citing this article, please also cite the underlying data sources. This article can be cited as:
Saloni Dattani (2023) - “How do researchers study the prevalence of mental illnesses?” Published online at OurWorldinData.org. Retrieved from: 'https://archive.ourworldindata.org/20251125-173858/how-do-researchers-study-the-prevalence-of-mental-illnesses.html' [Online Resource] (archived on November 25, 2025).BibTeX citation
@article{owid-how-do-researchers-study-the-prevalence-of-mental-illnesses,
author = {Saloni Dattani},
title = {How do researchers study the prevalence of mental illnesses?},
journal = {Our World in Data},
year = {2023},
note = {https://archive.ourworldindata.org/20251125-173858/how-do-researchers-study-the-prevalence-of-mental-illnesses.html}
}Reuse this work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
All of our charts can be embedded in any site.