How are causes of death registered around the world?
In many countries, when people die, the cause of their death is officially registered in their country’s national system. How is this determined?
To guide decisions in public health – whether that’s by governments, organizations, or individuals – it’s vital to know what people are dying from.
This helps us understand which conditions are going untreated, or how much investment is needed to address diseases; to see how much progress we’re making, and whether new challenges are emerging.
The ideal way to find out is by aggregating knowledge of the causes of death from medical professionals who know about each patient, their medical conditions and risk factors, and the circumstances in which they died.
But officially registering a death, and attributing a cause to it, can be difficult and complex. The process is affected by legal and cultural norms, access to healthcare, and advances in medical knowledge. Because of this, in many countries a large share of deaths are not registered at all.
How do medical practitioners identify the cause of death? How is the cause of death officially certified and registered? Why are these procedures lacking in many parts of the world? In this article, I summarise the answers to these questions.
In the additional information section, I also explain how researchers attribute the cause of death in countries where death registration is limited.
How is the cause of a death officially registered?
In many countries, when someone dies the cause of their death is determined by the medical practitioner who cared for them (such as a physician or nurse), or a coroner.
They look at evidence from the circumstances of the death, and use their medical knowledge and guidelines to certify the cause of death on a certificate.
The World Health Organization (WHO) provides international guidelines called the International Classification of Diseases (ICD) to guide practitioners on how the cause of death should be described. Death certificates in most countries are structured to follow these guidelines.
You can see two examples in this illustration.
In each example, the cause of death shown in death certificates is split into two parts.
In Part I, the medical practitioner or coroner has to list the chain of events that led to the death. They can use up to four lines, but don’t need to fill them all.
This includes the ‘immediate cause of death’ on the first line. Then, the next line contains the disease, injury, or condition that led to the immediate cause of death; and so on, until the lowest line contains the ‘underlying cause of death’.2
In Part II, the medical practitioner or coroner also lists other diseases, injuries, or conditions that contributed significantly to the death.
This should be done to the best of their knowledge, and as specifically as possible, but they can use words like ‘probable’ or ‘presumed’ when there is still uncertainty about the direct or underlying causes.
These considerations are important because the information they provide is then used to determine the ICD code of the cause of death using the ICD guidelines. These codes can help researchers analyze the data easily later on.3 Researchers can, for example, estimate the total number of people that died from tuberculosis using the specific ICD code A15.
This coding step may be done automatically, using a software program, or manually by a person.4 It is then stored in the country's vital registration system. Every year, each country reports its statistics on the causes of death to the WHO, by age and sex.5
What happens when a death is caused by multiple factors?
When researchers try to estimate the number of deaths caused by each factor, they tend to define each death as being caused by a single underlying cause of death. That’s what’s listed on death certificates.
But there are often other factors that contribute too, such as diseases, injuries and behavioral or environmental risk factors.
This is why death certificates include ‘other significant conditions’ that contributed to the death. Health practitioners or coroners can list these additional causes on death certificates if they have the relevant evidence surrounding the person's death, guidance, and medical knowledge.
Some behaviors – such as substance abuse (including alcoholism and chronic smoking) – are usually thought of as risk factors, but they also have ICD death codes. Doctors can list them on the death certificate as the underlying cause of death if they think this is the case.3
But doctors may not be certain about other risk factors that contributed to their death.
For example, air pollution increases people's risk of death by increasing their chances of developing lung diseases. However, the impact of air pollution on death is indirect and difficult to pinpoint for each individual. It does not have an ICD death code.
Another example is that age increases the risk of many diseases and conditions. However, ‘old age’ should not be listed on a death certificate as the underlying cause of death, because it is unspecific.
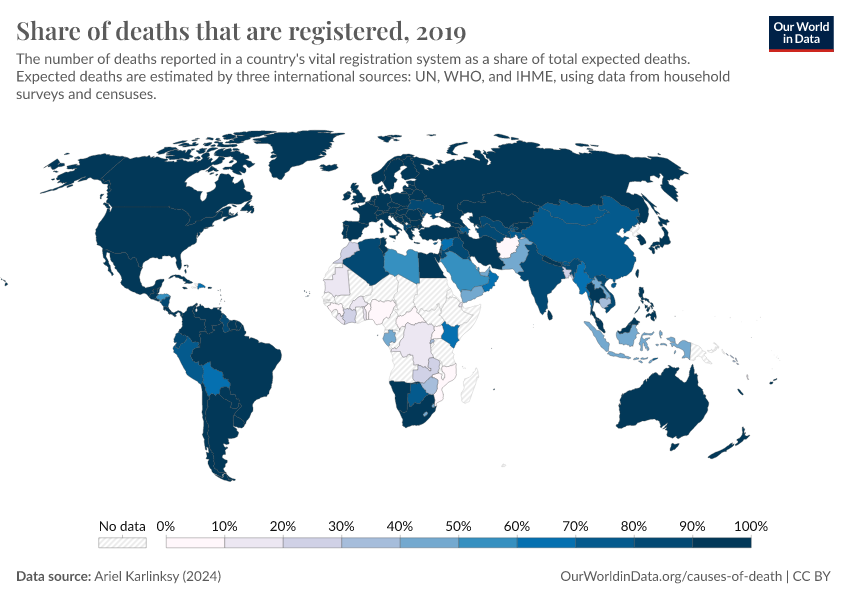
What share of deaths are registered?
The entire process of registering a death, and attributing a cause to it is not followed everywhere. One reason for this is that the entire vital registration system in the country may be absent or functioning poorly. This is especially true in low-income countries.
This means that, in many countries, most deaths are not registered at all. The chart shows that in some places, particularly across Africa, only a small share of deaths are registered.6
What share of deaths are attributed a cause?
Even in countries with a functioning vital registration system, someone's death may be registered without a cause.
This happens for several reasons.
There may not have been a health practitioner who cared for them, or a coroner to investigate and certify their death.
The person who died may not have come into contact with a medical professional or the healthcare system at all – for example, they may have died at home, which is more common in poorer countries.7
And even if a cause of death is determined, it may not have been coded into an ICD death code in the vital registration system.
In the chart here, you can see the share of total deaths that are officially registered with a cause of death.8
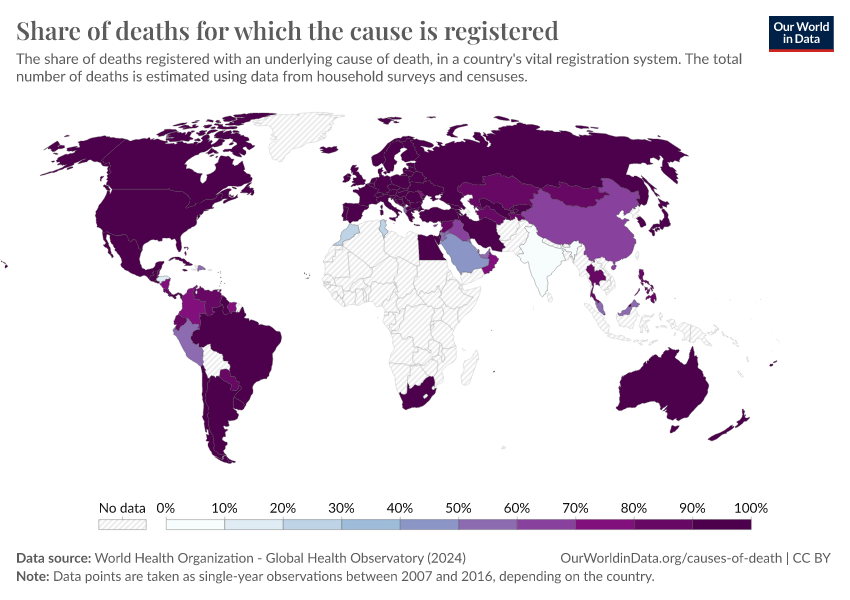
In many countries, the vast majority of deaths are registered with a cause of death. But in others, especially in Africa and South Asia, it’s only a small fraction.
Many countries are shown as having no data. This includes countries which don’t have a vital registration system, or have one that is poorly functioning.
Much of the world’s population lives in countries where only a small share of deaths are registered with a cause of death.
For example, in 2016, only a fifth of the world’s population – around 1.5 billion people – lived in countries where nearly all deaths were registered with a cause of death.
Which factors affect the choice of cause of death?
Even when deaths are registered with a cause of death, several factors can influence which cause of death is registered.
Some of these are related to the procedure of filling out a death certificate or coding the death. For example, physicians may not have had enough training, or the same training, in how to fill out the death certificate.1 The procedure of coding the information from a death certificate into an ICD code may also vary between hospitals, regions, or governments.
There are also legal or cultural factors. For example, relatives, caregivers, or others may hide evidence that may be relevant, particularly for causes of death that are stigmatized, such as suicide. In some countries, suicide is illegal and not even allowed as an option on the death certificate.9
Finally, there may be a lack of relevant evidence or hospital records for the deceased person. For example, they may not have been tested for the condition that led to their death, such as a particular infectious disease or cancer.
These factors can vary between countries and over time when there are changes in norms, medical knowledge, testing equipment, healthcare professionals, or coding practices.10
What are ill-defined causes of death, or ‘garbage codes’?
‘Garbage codes’ refer to a specific group of ICD codes. These contain causes of death that are ill-defined or often incorrectly coded.11
The cause of death may be given an ill-defined ICD code when there is a lack of evidence, testing, or hospital records on the person's death.
Some examples of ill-defined ICD codes include ‘sudden death’, ‘chest pain’, ‘heart failure’, ‘events of undetermined intent’, ‘cancer of unknown primary site’, and 'unspecified sepsis’.
These are considered garbage codes because they are not specific, and refer to the immediate cause of death or the symptoms preceding it, rather than the underlying cause.
They also provide little information, because it is common for people to die from a cause within those broad categories.12
On the chart, you can see the share of deaths registered with an ill-defined cause of death across countries.

Because of this problem, the IHME’s Global Burden of Disease (GBD) and the WHO's Global Health Estimates (GHE) both re-assign deaths with garbage codes to other ICD codes that are more specific or more likely, based on other data that is available.13
For example, deaths due to ‘cancer of unknown primary site’ may be re-assigned to specific cancer deaths according to how common those types of cancer deaths tend to be in previous research, and by using other information available about the person.
Conclusion
To reduce global mortality and improve healthcare, we need to know what people die from. While a lot of countries have good death registration systems, much of the world lives in countries where these systems are poor.
Researchers can use other methods to understand the causes of deaths, like verbal autopsies, but these also have limitations. These are explained in the ‘Additional Information’ section below.
If we want to understand what people are dying from, and reduce preventable deaths, we need better-functioning vital registration systems, medical records, and training for doctors and nurses to collect data where it’s lacking.
Endnotes
Brooks, E. G., & Reed, K. D. (2015). Principles and Pitfalls: A Guide to Death Certification. Clinical Medicine & Research, 13(2), 74–82. https://doi.org/10.3121/cmr.2015.1276
The underlying cause of death is defined by the WHO as: a) the disease or injury which initiated the train of morbid events leading directly to death, or b) the circumstances of the accident or violence which produced the fatal injury.
Brooks, E. G., & Reed, K. D. (2015). Principles and Pitfalls: A Guide to Death Certification. Clinical Medicine & Research, 13(2), 74–82. https://doi.org/10.3121/cmr.2015.1276
Also, coding may be done at a decentralized level (such as at a hospital) or centralized (at the regional or national level).
World Health Organization. (2020). WHO methods and data sources for country-level causes of death 2000-2019. https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_cod_methods.pdf?sfvrsn=37bcfacc_5&ua=1
Karlinsky, A. (2024). International completeness of death registration. Demographic Research, 50, 1151–1170. https://doi.org/10.4054/DemRes.2024.50.38
Adair, T. (2021). Who dies where? Estimating the percentage of deaths that occur at home. BMJ Global Health, 6(9), e006766. https://doi.org/10.1136/bmjgh-2021-006766
Total deaths are estimated by looking at the number of deaths expected to occur in the population in that year, based on the country’s demography.
Osafo, Joseph, Kwaku Oppong Asante, and Charity Sylvia Akotia. “Suicide Prevention in the African Region.” Crisis 41, no. Supplement 1 (March 1, 2020): S53–71. https://doi.org/10.1027/0227-5910/a000668. Rezaeian, Mohsen, and Murad Moosa Khan. “Suicide Prevention in the Eastern Mediterranean Region.” Crisis 41, no. Supplement 1 (March 1, 2020): S72–79. https://doi.org/10.1027/0227-5910/a000669. Snowdon, John, and Namkee G. Choi. “Undercounting of Suicides: Where Suicide Data Lie Hidden.” Global Public Health 15, no. 12 (December 1, 2020): 1894–1901. https://doi.org/10.1080/17441692.2020.1801789.
To adjust for changes when the entire ICD guidelines are revised, some researchers use 'bridge coding' methods to translate ICD codes used for older deaths to new codes. Brocco, S., Vercellino, P., Goldoni, C. A., Alba, N., Gatti, M. G., Agostini, D., Autelitano, M., Califano, A., Deriu, F., Rigoni, G., & others. (2010). «Bridge Coding» ICD-9, ICD-10 and effects on mortality statistics. Epidemiologia e Prevenzione, 34(3), 109–119.
Another problem is when deaths are coded with an ICD code that is incorrect due to legal or cultural factors.
For example, in some countries, suicide may be given an incorrect cause of death due to its stigmatization. Instead, these deaths may be incorrectly listed as caused by 'events of undetermined intent', accidents, homicides, or unknown causes. See: Snowdon, J., & Choi, N. G. (2020). Undercounting of suicides: Where suicide data lie hidden. Global Public Health, 15(12), 1894–1901. https://doi.org/10.1080/17441692.2020.1801789
Both types of garbage codes cause problems for health studies, where researchers need good data on the number of deaths caused by a given factor. In these cases, for example, a fraction of deaths that are officially due to 'events of undetermined intent', accidents, or unknown causes, may be re-assigned to suicide. This can adjust for the underreporting and misclassification of suicide deaths in many countries.
Ellingsen, C. L., Alfsen, G. C., Ebbing, M., Pedersen, A. G., Sulo, G., Vollset, S. E., & Braut, G. S. (2022). Garbage codes in the Norwegian Cause of Death Registry 1996–2019. BMC Public Health, 22(1), 1301. https://doi.org/10.1186/s12889-022-13693-w
Naghavi, M., Richards, N., Chowdhury, H., Eynstone-Hinkins, J., Franca, E., Hegnauer, M., Khosravi, A., Moran, L., Mikkelsen, L., & Lopez, A. D. (2020). Improving the quality of cause of death data for public health policy: Are all ‘garbage’ codes equally problematic? BMC Medicine, 18(1), 55. https://doi.org/10.1186/s12916-020-01525-w
World Health Organization. (2020). WHO methods and data sources for country-level causes of death 2000-2019. https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_cod_methods.pdf?sfvrsn=37bcfacc_5&ua=1
Naghavi, M. (2019). Global, regional, and national burden of suicide mortality 1990 to 2016: Systematic analysis for the Global Burden of Disease Study 2016. BMJ, l94. https://doi.org/10.1136/bmj.l94
The WHO has a standard verbal autopsy structure that can be used routinely by countries. World Health Organization. (2022). Verbal autopsy standards: The 2022 WHO verbal autopsy instrument. https://cdn.who.int/media/docs/default-source/classification/other-classifications/autopsy/2022-va-instrument/verbal-autopsy-standards_2022-who-verbal-autopsy-instrument_v1_final.pdf?sfvrsn=c8cf2dda_8
In some countries, verbal autopsies have been conducted as part of representative surveys. Rahman, A. E., Hossain, A. T., Siddique, A. B., Jabeen, S., Chisti, M. J., Dockrell, D. H., Nair, H., Jamil, K., Campbell, H., & El Arifeen, S. (2021). Child mortality in Bangladesh - why, when, where and how? A national survey-based analysis. Journal of Global Health, 11, 04052. https://doi.org/10.7189/jogh.11.04052 But this is not always the case; they are often conducted in only some regions within countries. WHO interactive map on the use of the WHO verbal autopsy instrument. https://www.who.int/standards/classifications/other-classifications/verbal-autopsy-standards-ascertaining-and-attributing-causes-of-death-tool This means researchers may not have an accurate or full picture of the causes of death across the country.
Thomas, L.-M., D’Ambruoso, L., & Balabanova, D. (2018). Verbal autopsy in health policy and systems: A literature review. BMJ Global Health, 3(2), e000639. https://doi.org/10.1136/bmjgh-2017-000639 Lawn, J. E., Osrin, D., Adler, A., & Cousens, S. (2008). Four million neonatal deaths: Counting and attribution of cause of death. Paediatric and Perinatal Epidemiology, 22(5), 410–416. https://doi.org/10.1111/j.1365-3016.2008.00960.x
An example of a nationwide health facility audit can be found here. Sayinzoga, F., Bijlmakers, L., van Dillen, J., Mivumbi, V., Ngabo, F., & van der Velden, K. (2016). Maternal death audit in Rwanda 2009–2013: A nationwide facility-based retrospective cohort study. BMJ Open, 6(1), e009734. https://doi.org/10.1136/bmjopen-2015-009734
Willcox, M. L., Price, J., Scott, S., Nicholson, B. D., Stuart, B., Roberts, N. W., Allott, H., Mubangizi, V., Dumont, A., & Harnden, A. (2020). Death audits and reviews for reducing maternal, perinatal and child mortality. Cochrane Database of Systematic Reviews, 2020(3). https://doi.org/10.1002/14651858.CD012982.pub2
Organization, W. H. & others. (2018). Improving the quality of paediatric care: An operational guide for facility-based audit and review of paediatric mortality. https://apps.who.int/iris/bitstream/handle/10665/279755/9789241515184-eng.pdf
Cite this work
Our articles and data visualizations rely on work from many different people and organizations. When citing this article, please also cite the underlying data sources. This article can be cited as:
Saloni Dattani (2023) - “How are causes of death registered around the world?” Published online at OurWorldinData.org. Retrieved from: 'https://archive.ourworldindata.org/20260119-070102/how-are-causes-of-death-registered-around-the-world.html' [Online Resource] (archived on January 19, 2026).BibTeX citation
@article{owid-how-are-causes-of-death-registered-around-the-world,
author = {Saloni Dattani},
title = {How are causes of death registered around the world?},
journal = {Our World in Data},
year = {2023},
note = {https://archive.ourworldindata.org/20260119-070102/how-are-causes-of-death-registered-around-the-world.html}
}Reuse this work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
All of our charts can be embedded in any site.