Antiretroviral therapy has saved millions of lives from AIDS and could save more
Since the late 1980s, antiretroviral therapy has already saved millions of lives from HIV/AIDS. But millions of people with HIV still aren’t getting this life-saving treatment.
38 million people had HIV/AIDS in 2020. A couple of decades ago, the chances of surviving more than ten years with HIV were slim. Today, thanks to antiretroviral therapy (ART), people with HIV/AIDS can expect to live long lives.
ART is a mixture of antiviral drugs that are used to treat people infected with human immunodeficiency virus (HIV). It is an essential player in making progress against HIV/AIDS because it saves lives, allows people with HIV to live longer, and prevents new HIV infections.
Millions of lives are saved by ART
Since the first version of ART was introduced in the late 1980s, the treatment has saved millions of lives.
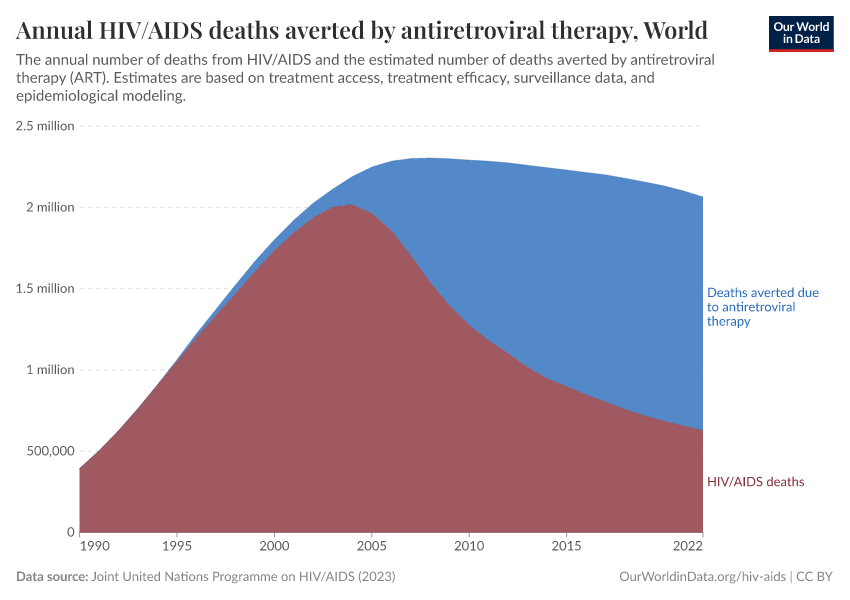
The chart here shows the annual number of deaths from HIV/AIDS and the number of deaths averted as a result of ART.
Globally, 1 million people died from HIV/AIDS in 2016, but even more deaths – 1.2 million – were averted as a result of ART. Without ART, more than twice as many people would have died from HIV/AIDS.
People who use ART are living longer
ART not only saves lives but also gives a chance for people living with HIV/AIDS to live long lives. Without ART very few infected people survive beyond ten years.1
Today, a person living in a high-income country who started ART in their twenties can expect to live for another 46 years — that is well into their 60s.2
While the life expectancy of people living with HIV/AIDS in high-income countries has still not reached the life expectancy of the general population, we are getting closer to this goal.3
The combination of antiretroviral drugs which make-up ART have progressively improved. Recent research shows that a person who started ART in the late 1990s would be expected to live ten years less than a person who started ART in 2008.4 This increase goes beyond the general increase in life expectancy in that period and reflects the improvements in ART — fewer side effects, more people following the prescribed treatment, and more support for the people in need of ART.
ART prevents new HIV infections
There is considerable evidence to show that people who use ART are less likely to transmit HIV to another person.5 ART reduces the number of viral particles present in an HIV-positive individual and therefore, the likelihood of passing the virus to another person decreases.
In 2011, the journal Science named a study that found that ART reduced the risk of HIV transmission between couples by 96% as its “Breakthrough of the Year”.6 Many other studies have now shown similar findings, with a range of reduction in transmission attributable to ART depending on location and groups studied.7 A study from British Columbia, for example, showed that with every 10% increase in ART coverage there was an 8% decrease in new diagnoses of HIV.8
We need to increase ART coverage
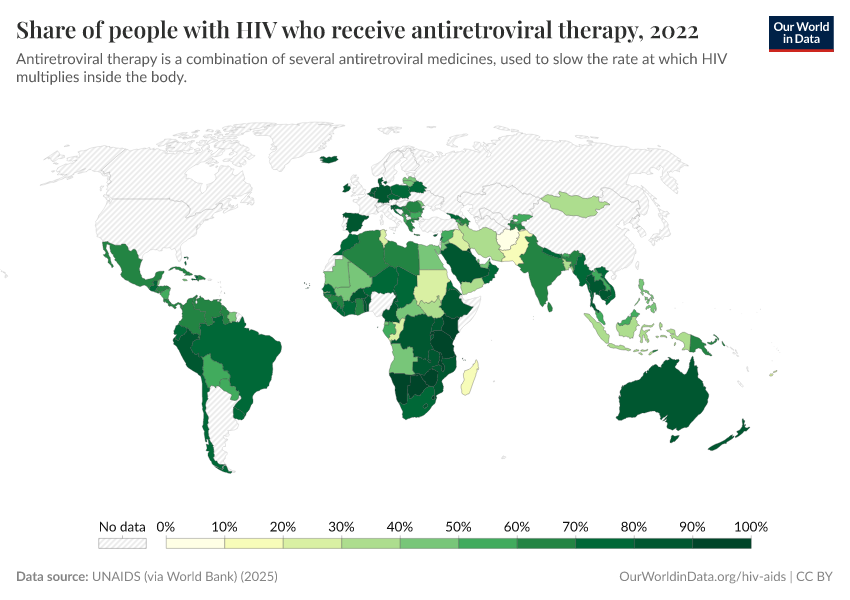
The number of people who receive ART has increased significantly in recent years, especially in African countries where the prevalence of HIV/AIDS is the highest. You can see this in the map. In 2005 only 2 million people received ART; by 2018 this figure has increased more than ten-fold to 23 million.9
But still, 23 million is only 61% of HIV-positive individuals. It means that 14.6 million people who could benefit from the life-saving treatment currently don’t.
To increase ART coverage we need to first improve access to testing for HIV status. In 2018, 79% of people living with HIV knew their status. This means 1-in-5 people living with HIV are unaware.10 And awareness is also not enough. In Sub-Saharan Africa among people who are HIV positive only 57% go on to complete required pre-treatment assessments.11 And of those who should start ART only 66% do.12
Stigmatization of people who have HIV/AIDS also leads to a decrease in engagement with care, treatment, and prevention services.13
Due to its success ART is sometimes called the Lazarus drug, referring to the biblical story about a man raised from the dead.14 With access to ART, HIV/AIDS is no longer a death sentence. But to make progress against HIV/AIDS and fully benefit from the potential of ART treatment we need to increase HIV/AIDS awareness and improve access to ART.
Endnotes
We should note, though, that the life expectancy for people living with HIV infection without ART can vary depending on the age when a person got infected with HIV, a person's immune status (e.g. CD4 count), and socioeconomic factors.
Babiker, A., Darby, S., De Angelis, D., Kwart, D., Porter, K., Beral, V., ... & Prins, M. (2000). Time from HIV-1 seroconversion to AIDS and death before widespread use of highly-active antiretroviral therapy: a collaborative re-analysis. Collaborative Group on AIDS Incubation and HIV Survival including the CASCADE EU Concerted Action. Concerted Action on SeroConversion to AIDS and Death in Europe. Lancet, 355(9210).
Wandel, S., Egger, M., Rangsin, R., Nelson, K. E., Costello, C., Lewden, C., ... & Minga, A. (2008). Duration from seroconversion to eligibility for antiretroviral therapy and from ART eligibility to death in adult HIV-infected patients from low and middle-income countries: collaborative analysis of prospective studies. Sexually transmitted infections, 84(Suppl_1), i31-i36.
This number is based on a study that used European and North American countries. Few studies have systematically assessed life expectancy of people living with HIV/AIDS in middle and low-income countries, but it is predicted to be significantly lower between 60-74% of the life expectancy of the general population (see Wandeler et al. reference).
Multiple factors account for this difference including higher prevalence of other diseases, such as co-infections with hepatitis or TB and higher prevalence of opportunistic diseases. In addition, people tend to adhere to ART regimen less strictly because of poorer care for AIDS patients, less access to medical clinics, and social stigma.
Wandeler, G., Johnson, L. F., & Egger, M. (2016). Trends in life expectancy of HIV-positive adults on ART across the globe: comparisons with general population. Current Opinion in HIV and AIDS, 11(5), 492.
For low and middle-income countries currently no equivalent estimate is available for life-expectancy. However, we do know that with decreasing rates of HIV mortality in low and middle-income countries the life expectancy of the general population has increased. Haris et al. reference discuss this and you can read more about life expectancy and HIV here.
Harris, T. G., Rabkin, M., & El-Sadr, W. M. (2018). Achieving the fourth 90: healthy aging for people living with HIV. AIDS (London, England), 32(12), 1563.
Trickey, A., May, M. T., Vehreschild, J. J., Obel, N., Gill, M. J., Crane, H. M., ... & Cavassini, M. (2017). Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies.The Lancet HIV, 4(8), e349-e356.
Global average life expectancy in 2019 was 72.6 years. The average life expectancy in Europe is 78.6 years.
Trickey, A., May, M. T., Vehreschild, J. J., Obel, N., Gill, M. J., Crane, H. M., ... & Cavassini, M. (2017). Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies.The Lancet HIV, 4(8), e349-e356.
G Williams, B., Lima, V., & Gouws, E. (2011). Modelling the impact of antiretroviral therapy on the epidemic of HIV.Current HIV research, 9(6), 367-382.
Science announcement:
Cohen, J. (2011). HIV treatment as prevention.
Study that was awarded:
Cohen, M. S., Chen, Y. Q., McCauley, M., Gamble, T., Hosseinipour, M. C., Kumarasamy, N., ... & Godbole, S. V. (2011). Prevention of HIV-1 infection with early antiretroviral therapy.New England journal of medicine, 365(6), 493-505.
PARTNER study showed chances of transmission between gay couples with successfull virus suppression by ART are “effectively zero”.
Rodger, A. J., Cambiano, V., Bruun, T., Vernazza, P., Collins, S., Degen, O., ... & Raben, D. (2019). Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study.The Lancet.
Transmission rates in Madrid fell by 86% after ART became available
Castilla, J., Del Romero, J., Hernando, V., Marincovich, B., García, S., & Rodríguez, C. (2005). Effectiveness of highly active antiretroviral therapy in reducing heterosexual transmission of HIV. JAIDS Journal of Acquired Immune Deficiency Syndromes, 40(1), 96-101.
A study in San Francisco showing after ART became available, viral loads dropped to 40% and HIV infection rates fell by 60%.
Das, M., Chu, P. L., Santos, G. M., Scheer, S., Vittinghoff, E., McFarland, W., & Colfax, G. N. (2010). Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PloS one, 5(6), e11068.
After ART became freely available in Taiwan transmission rates fell by 50%. Fang, C. T., Hsu, H. M., Twu, S. J., Chen, M. Y., Chang, Y. Y., Hwang, J. S., ... & Division of AIDS and STD, Center for Disease Control, Department of Health, Executive Yuan. (2004). Decreased HIV transmission after a policy of providing free access to highly active antiretroviral therapy in Taiwan.Journal of Infectious Diseases, 190(5), 879-885.
Hogg, R. S., Heath, K., Lima, V. D., Nosyk, B., Kanters, S., Wood, E., ... & Montaner, J. S. (2012). Disparities in the burden of HIV/AIDS in Canada. PLoS One, 7(11), e47260.
Source. https://www.who.int/gho/hiv/epidemic_response/ART/en/
The 79% figure is based on 2019 UNAIDS estimates.
The frequency of undiagnosed HIV/AIDS can be measured using observational studies. Measures of expected rate of HIV infection, the actual number of people diagnosed with HIV and delay in diagnosis are taken into account to predict the true expected prevalence of HIV in a population and the proportion of undiagnosed cases (see Singh et al. reference).
The initial HIV infection is often followed by flu-like symptoms, which subside in a couple of weeks. The infected patient can then go on to live without any symptoms for months or years while their immune system may be slowly deteriorating. Hence, people infected with HIV may not even know they need to be tested due to the lack of symptoms. Models used to predict HIV incidence rate often use an expected 5 year lag between infection and diagnosis.
Singh, S., Song, R., Johnson, A. S., McCray, E., & Hall, H. I. (2018). HIV incidence, prevalence, and undiagnosed infections in US men who have sex with men.Annals of internal medicine, 168(10), 685-694.
WHO eligibility criteria are based on the so called CD4 counts, which go down as the illness progresses. Healthy person’s CD4 counts are >500/mm3. WHO recommends ART for anyone with HIV diagnosis and CD4 count >350 cells and ≤500/mm3, regardless of clinical symptoms. All children, people with TB, HBV, and pregnant women diagnosed with HIV regardless of their CD4 status should get ART. https://www.who.int/hiv/pub/guidelines/arv2013/art/statartadolescents/en/
Kranzer, K., Govindasamy, D., Ford, N., Johnston, V., & Lawn, S. D. (2012). Quantifying and addressing losses along the continuum of care for people living with HIV infection in sub‐Saharan Africa: a systematic review.Journal of the International AIDS Society, 15(2), 17383.
For some countries eligibility for ART treatment is determined by the so called CD4+ counts, which go down as the illness progresses.
Kranzer, K., Govindasamy, D., Ford, N., Johnston, V., & Lawn, S. D. (2012). Quantifying and addressing losses along the continuum of care for people living with HIV infection in sub‐Saharan Africa: a systematic review.Journal of the International AIDS Society, 15(2), 17383.
Mahajan, A. P., Sayles, J. N., Patel, V. A., Remien, R. H., Ortiz, D., Szekeres, G., & Coates, T. J. (2008). Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS (London, England), 22(Suppl 2), S67.
Tompsett, A. (2019). The Lazarus drug the impact of antiretroviral therapy on economic growth. Journal of Development Economics, 102409.
Flynn, M. B. (2014). Pharmaceutical autonomy and public health in Latin America: State, society and industry in Brazil’s AIDS program. Routledge.
Cite this work
Our articles and data visualizations rely on work from many different people and organizations. When citing this article, please also cite the underlying data sources. This article can be cited as:
Bernadeta Dadonaite (2019) - “Antiretroviral therapy has saved millions of lives from AIDS and could save more” Published online at OurWorldinData.org. Retrieved from: 'https://archive.ourworldindata.org/20260112-111535/art-lives-saved.html' [Online Resource] (archived on January 12, 2026).BibTeX citation
@article{owid-art-lives-saved,
author = {Bernadeta Dadonaite},
title = {Antiretroviral therapy has saved millions of lives from AIDS and could save more},
journal = {Our World in Data},
year = {2019},
note = {https://archive.ourworldindata.org/20260112-111535/art-lives-saved.html}
}Reuse this work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
All of our charts can be embedded in any site.