How new vaccines can help with our antibiotic dependence
This article is outdated
This article was published in 2017 and has not been updated to reflect new vaccines that have been introduced since then.
Antibiotics are antimicrobial drugs used to kill bacteria. Along with vaccines, antibiotics often top lists of the most important medical discoveries, with both interventions having a tremendous impact on illness and deaths from communicable diseases.1
However, the usefulness of antibiotics to medicine is under threat. A national campaign in the UK called ‘Keep Antibiotics Working’ is trying to prevent antibiotic misuse and overuse by making the point that antibiotics are useless for many illnesses that they are asked for (for example, viral infections such as cold or flu) and contribute to the 5,000 deaths a year in England from untreatable illnesses.
Still it is poorer countries across the world that are likely to take the biggest toll from antibiotic-resistant infections. In 2014 a UK study predicted that by 2050 the African region will account for 4.15 million deaths a year attributable to antibiotic-resistant infections and the Asian region 4.73 million. The World Health Organization (WHO) is pursuing a similar campaign this week encouraging all countries to think about antibiotic resistance for ‘World Antibiotic Awareness Week’. The theme this year is: 'Seek advice from a qualified healthcare professional before taking antibiotics'.
Vaccines as a solution for antimicrobial resistance
Increasing resistance could make common interventions of modern medicine, such as surgery, chemotherapy, and caesarean sections too dangerous to carry out. As England's Chief Medical Officer Dame Sally Davies already warned in 2013:“Antimicrobial resistance poses a catastrophic threat. If we don’t act now, any one of us could go into hospital in 20 years for minor surgery and die because of an ordinary infection that can’t be treated by antibiotics.”
One means of slowing antimicrobial resistance is by combating misuse and overuse as proposed by the campaigns ‘Keep Antibiotics Working’ and 'Seek advice from a qualified healthcare professional before taking antibiotics'. Other measures include encouraging better hygiene and infection control, surveillance of drug resistance, and reducing the overuse of antibiotics for livestock in agriculture (we at OWID looked at this issue in last week's post).
Another option is to foster scientific discovery, in order to produce new antibiotics or diagnostics to analyze whether antibiotics are indeed needed. New vaccines are not often connected with solutions for antimicrobial resistance. But vaccine resistance compared with antimicrobial resistance is rare. With a vaccination there is less time for the pathogen to evolve as the body is ready to fight off the infection and also because vaccines target many structures of the pathogen, while antimicrobial drugs target one specific part of the pathogen so that just one mutation can result in resistance.2 Vaccines therefore present opportunities to reduce our dependence on antibiotics. They can do this in two ways:
- Vaccines against bacterial diseases reduce the number of infections and antibiotics used as treatment, including the spectrum of antibiotics used for a condition like pneumonia.3 This effect can be enhanced by herd immunity where protection is extended to unvaccinated persons in the population. The most used vaccinations for bacteria are for diphtheria, tetanus and pertussis, usually combined into one injection (DTP).
- Vaccines against viral diseases such as the influenza vaccine reduce the number of infections that are then mistreated with antibiotics. A US study showed that antibiotics were inappropriately prescribed for 79% of influenza patients, with estimated costs of $211 million annually.4 Furthermore any other complications from a vaccine-preventable disease such as surgery or bacterial infection acquired because of a weakened immune system or hospital stay could also be avoided. A Canadian study estimated a reduction of 60% for antibiotic prescriptions during the influenza season after introduction of a universal seasonal influenza immunization program.5
Vaccines that are particularly worth scaling up are for pneumococcus and Haemophilus influenzae type b (Hib), to tackle the approximately 935,000 worldwide of under-5 deaths from pneumonia each year, with these vaccines not yet sufficiently deployed in China, India, Nigeria, Bangladesh, Afghanistan and Indonesia.6 Laxminarayan et al. estimate that for children under 5 years, this amounts to a 47% reduction in days on antibiotics per year with a pneumococcal conjugate vaccine (PCV) that can prevent pneumonia. They estimate that 11.4 million days of antibiotics could be saved in the 75 countries included in their analysis.
How new vaccines can help
No vaccines are currently available for the three bacteria highlighted by the US Centers for Disease Control and Prevention (CDC) as an ‘urgent’ hazard of developing resistance (Clostridium difficile, Carbapenem-resistant Enterobacteriaceae or CRE and drug-resistant Neisseria gonorrhoeae).7 The CDC lists 11 bacteria and one fungus at the 'serious' hazard level, and three bacteria at the 'concerning' hazard level.
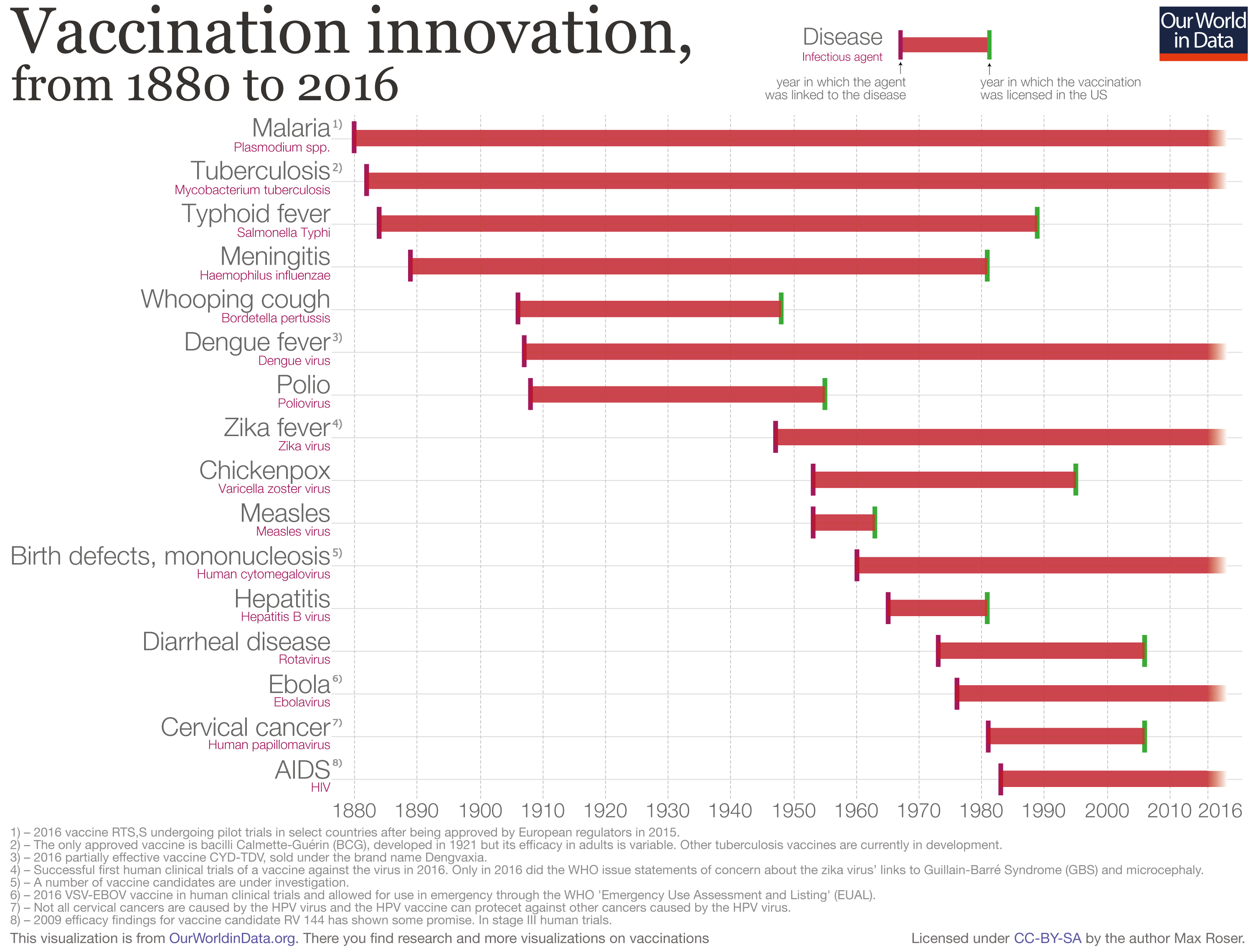
As our visualization below shows, new vaccines tend to take a long time and vast resources to develop. However, it could be an investment that is worth making, as the problem of antimicrobial resistance does not affect vaccines. Bacterial diseases routinely vaccinated against for decades, for example diphtheria and pertussis, have not shown significant resistance against antibiotics and also resistance for other diseases has been reversed after the vaccine was introduced.8
A bacteria that the CDC listed as at a serious hazard level was drug-resistant Salmonella typhi, causing typhoid fever (simply known as typhoid). Typhoid is a bacterial disease that infects over 12 million people worldwide each year. The two current vaccines that are available are not suitable for young children nor protective for long periods of time, plus multi-drug-resistant typhoid has been on the rise.
A new vaccine for typhoid, tested successfully by the Oxford Vaccine Group at the University of Oxford could help reduce dependence on antibiotics. The new typhoid conjugate vaccine (TCV) is suitable for children under two and offers longer lasting protection. Gavi, the international organisation that funds vaccines in low and middle-income countries, is now considering backing the vaccine. The chief executive of Gavi, Dr Seth Berkley has stated: “Not only could this vaccine save lives, it could also prove to be a valuable weapon in the fight against antimicrobial resistance.”
We need to pursue a wide range of options in order to deal with antimicrobial resistance, including new vaccines. The TCV for typhoid is a step in this direction.
Endnotes
Armstrong, G. L., Conn, L. A. and Pinner, R. W. (1999) – Trends in infectious disease mortality in the United States during the 20th Century, Journal of the American Medical Association, 281, 61-66. Available here
Kennedy DA, Read AF. 2017. Why does drug resistance readily evolve but vaccine resistance does not? Proc. R. Soc. B 284: 20162562. http://dx.doi.org/10.1098/rspb.2016.2562 Available here
Lipsitch M, Siber GR. 2016. How can vaccines contribute to solving the antimicrobial resistance problem? mBio 7(3):e00428-16. doi:10.1128/mBio.00428-16. Available online
Source. https://www.ncbi.nlm.nih.gov/pubmed/27273824
Jeffrey C. Kwong, Sarah Maaten, Ross E. G. Upshur, David M. Patrick, Fawziah Marra; The Effect of Universal Influenza Immunization on Antibiotic Prescriptions: An Ecological Study, Clinical Infectious Diseases, Volume 49, Issue 5, 1 September 2009, Pages 750–756, https://doi.org/10.1086/605087 Available online
Laxminarayan, Ramanan et al. (2016) – Access to effective antimicrobials: a worldwide challenge. The Lancet Volume 387, Issue 10014, 168 – 175. Available here.
Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United States, 2013. Atlanta: CDC; 2013. Available online
Lipsitch, Marc, and George R. Siber. 2016. “How Can Vaccines Contribute to Solving the Antimicrobial Resistance Problem?” mBio 7 (3): e00428-16. doi:10.1128/mBio.00428-16. http://dx.doi.org/10.1128/mBio.00428-16. Available online
Cite this work
This content is outdated, but if you would still like to use it, here is how to cite it:
Our articles and data visualizations rely on work from many different people and organizations. When citing this article, please also cite the underlying data sources. This article can be cited as:
Samantha Vanderslott (2017) - “How new vaccines can help with our antibiotic dependence” Published online at OurWorldinData.org. Retrieved from: 'https://ourworldindata.org/vaccines-antibiotic-dependence' [Online Resource]BibTeX citation
@article{owid-vaccines-antibiotic-dependence,
author = {Samantha Vanderslott},
title = {How new vaccines can help with our antibiotic dependence},
journal = {Our World in Data},
year = {2017},
note = {https://ourworldindata.org/vaccines-antibiotic-dependence}
}All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.